Vaginal Yeast Infections: Symptoms, Causes and Treatment
Introduction
Vaginal yeast infections, commonly known as thrush, are a prevalent health issue affecting many women across various stages of life. These infections are often marked by discomforting symptoms such as itching, burning sensations, and abnormal vaginal discharge. In some instances, a yeast infection might not present any noticeable symptoms, making it challenging to detect without medical evaluation.
A vaginal yeast infection occurs when there is an overgrowth of yeast, specifically a type of fungus known as Candida, in the vaginal area. This overgrowth leads to inflammation and irritation. Alongside bacterial infections, yeast infections are among the most common causes of vaginal inflammation and irritation.
The condition is particularly common among women during certain life phases such as pregnancy, and several factors can increase susceptibility. Fortunately, effective treatments are available and can help alleviate symptoms, often through the use of vaginal suppositories, topical creams, or oral medications if needed.
Key Points at a Glance
- Symptoms: Common symptoms include itching, burning, and a white or yellowish discharge.
- Causes: The primary cause is an overgrowth of Candida albicans, a type of yeast normally found in the vaginal flora.
- Risk Factors: Hormonal changes, a weakened immune system, and certain medications increase susceptibility.
- Treatment: Typically involves antifungal vaginal suppositories or creams, with oral tablets used for more severe or persistent cases.
Vaginal Yeast Infection Symptoms
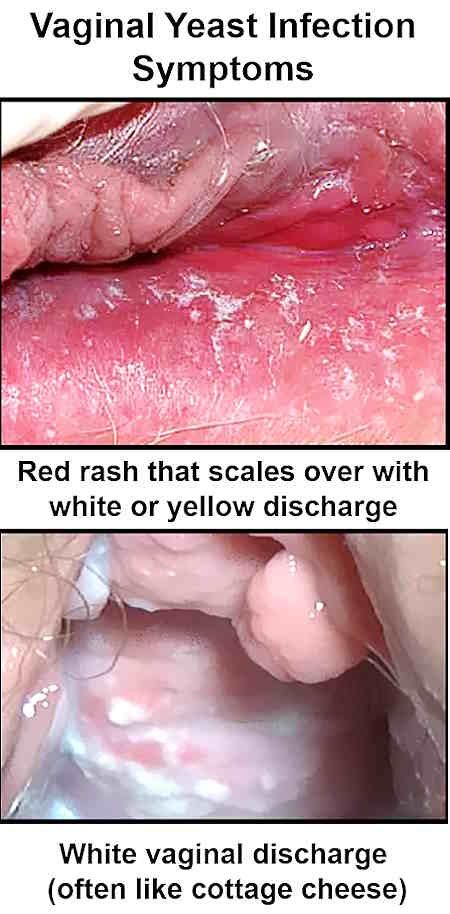
Vaginal yeast infections can present with a variety of symptoms that significantly impact a woman’s comfort and quality of life:
- Itching and Burning: One of the most prevalent symptoms, itching and burning sensations are often localized to the vaginal area and can extend to the external genitals.
- Pain: Women may experience pain during sexual intercourse or while urinating. This discomfort is a result of inflammation and irritation in the vaginal tissues.
- Discharge: A characteristic white or yellowish discharge is common, often described as having a consistency similar to curdled milk or cottage cheese. This discharge can be either chunky or watery.
- External Irritation: The labia (the outer lips of the vagina) may become red and swollen. Symptoms may worsen in the days leading up to menstruation.
Vaginal yeast infection symptoms can vary in severity and may significantly affect daily activities and overall well-being.
Vaginal Yeast Infection Causes and Risk Factors
Understanding the causes and risk factors associated with vaginal yeast infections can help in prevention and management.
- Yeast Overgrowth: Vaginal yeast infections are primarily caused by an overgrowth of Candida albicans, a yeast that is normally present in small amounts within the vaginal environment. Under normal conditions, the balance between various microorganisms in the vagina keeps Candida levels in check. However, an imbalance can lead to overgrowth and infection.
- Hormonal Changes: Hormonal fluctuations play a significant role in the development of yeast infections. During pregnancy, the body experiences a surge in estrogen levels, which can disrupt the natural balance of vaginal microorganisms. Similarly, hormonal changes caused by the contraceptive pill can increase the likelihood of developing yeast infections.
- Medical Conditions: Certain medical conditions, particularly those affecting the immune system, can increase susceptibility to yeast infections. Diabetes, for example, can create an environment conducive to yeast overgrowth due to elevated blood sugar levels. Other immune-compromising conditions or treatments, such as those used in cancer therapy, can also increase the risk.
- Medications: Various medications, including antibiotics, steroids, and hormone therapies, can alter the balance of vaginal flora, making it easier for yeast to proliferate. Antibiotics, in particular, can disrupt the natural balance of bacteria and yeast in the vagina.
- Lifestyle Factors: Stress, excessive washing with soaps, and wearing tight or non-breathable clothing can also contribute to the development of yeast infections. These factors can create an environment where yeast thrives, leading to infection.
- Sexual Transmission: Although a vaginal yeast infection is not classified as a sexually transmitted disease (STD), it can still be transmitted through sexual activity. For example, if a sexual partner has a yeast infection, the yeast may be introduced into the vagina during intercourse, potentially leading to an infection.
Prevalence and Outlook
Yeast infections are the second most common cause of vaginal inflammation, with bacterial infections being the most common. It is estimated that up to 75% of women will experience a vaginal yeast infection at least once in their lifetime. These infections are particularly prevalent among women of childbearing age.
Postmenopausal women may also experience yeast infections, often related to hormonal treatments such as estrogen replacement therapy. The symptoms of yeast infections are often mild and can sometimes be absent altogether. Severe cases are relatively rare and usually require more intensive treatment.
Frequent or recurrent yeast infections may necessitate further investigation to identify underlying conditions that may be contributing to the problem. Persistent infections, particularly in the context of a weakened immune system, may require more aggressive treatment and management strategies.
Effects of Vaginal Yeast Infections
- Complications: While serious complications are rare, they can occur, particularly in individuals with compromised immune systems. Conditions such as cancer or AIDS can exacerbate yeast infections and lead to more severe complications. In pregnant women, yeast infections may slightly increase the risk of complications such as premature labor, miscarriage, or preterm birth. Additionally, yeast infections can be transmitted to newborns during delivery, potentially causing diaper rash or oral thrush in the infant.
- Impact on Daily Life: Many women may feel embarrassed about discussing genital health issues, leading to delays in seeking treatment. This can exacerbate symptoms and increase the risk of transmission to sexual partners. It is important for women to address symptoms promptly and communicate openly with their healthcare providers.
Diagnosis of Vaginal Yeast Infections
Diagnosing a vaginal yeast infection typically involves a combination of evaluating symptoms and conducting a physical examination. The healthcare provider may inspect the vaginal lining for signs of infection. If there is uncertainty about the diagnosis, a sample of vaginal discharge may be collected and examined under a microscope for the presence of yeast cells.
In cases of recurrent or severe infections, additional testing may be necessary to identify underlying risk factors or conditions. It may also be beneficial for partners to be evaluated if they exhibit symptoms of a genital yeast infection.
Prevention Strategies
- For Individuals with Weakened Immune Systems: Antifungal medications may be prescribed as a preventive measure against fungal infections. This approach can help reduce the risk of developing yeast infections in individuals with compromised immune systems.
- Healthy Practices: Maintaining good hygiene and avoiding irritants such as douches or scented hygiene products is crucial in preventing yeast infections. Wearing breathable clothing and managing stress are also important for maintaining a healthy vaginal environment.
- Probiotics: The use of probiotics for preventing yeast infections remains a topic of ongoing research. Probiotics aim to restore or promote a healthy balance of microorganisms in the vagina but should be used with caution.
- Avoidance of Risk Factors: Reducing exposure to risk factors such as excessive stress, tight clothing, and certain hygiene products can help prevent yeast infections.
Vaginal Yeast Infection Treatment / Medication
- Antifungal Medications: The most common treatment for vaginal yeast infections involves antifungal medications. These can be administered in the form of vaginal suppositories or creams. Treatment usually lasts between 1 to 6 days, depending on the specific product used. While these treatments are effective, they can sometimes cause temporary side effects such as burning or itching.
- Oral Medications: For more severe or persistent infections, oral antifungal tablets may be prescribed. However, these medications can interact with other drugs and may cause side effects such as nausea, diarrhea, or headache. Oral antifungal medications are not recommended for use during pregnancy.
- Alternative Remedies: Some women may use home remedies such as garlic cloves, tea tree oil-soaked tampons, or natural yogurt to address yeast infections. However, there is limited research supporting the effectiveness and safety of these treatments. Possible risks include allergic reactions and irritation.
- Probiotics: Suppositories or capsules containing live lactic acid bacteria (probiotics) may be used to help restore the natural balance of vaginal flora. The effectiveness of these treatments is still under investigation.
- Avoiding Vaginal Douches: Vaginal douches should be avoided, as they can disrupt the natural balance of microorganisms in the vagina and potentially worsen symptoms.
Frequently Asked Questions (FAQs)
Do probiotics help prevent vaginal yeast infections?
There is some evidence to suggest that probiotics, particularly strains like Lactobacillus acidophilus, may help prevent yeast infections. However, the research is mixed regarding their effectiveness as a reliable preventive measure or treatment. While some studies show benefits, others are inconclusive, making it important to consult with a healthcare provider for personalized advice.
How do vaginal yeast infections affect pregnancy?
Pregnancy increases the likelihood of developing a vaginal yeast infection. During pregnancy, the treatment approach may differ. Healthcare providers generally recommend topical treatments, such as vaginal creams or suppositories, as these are considered safer during pregnancy. Oral treatments like fluconazole are typically avoided in the first trimester but may be used if necessary later in pregnancy. Always consult your doctor for guidance on the safest treatment options during pregnancy.
Can someone get more vaginal yeast infections while menstruating?
Hormonal changes that occur during menstruation can make yeast infections more likely. This is why some individuals might experience worsening symptoms or develop a yeast infection just before their period starts. Conversely, menstruation may sometimes help clear up a yeast infection, as the higher pH of menstrual blood can help restore the vaginal pH balance.
Can a vaginal yeast infection go away on its own?
While some mild yeast infections might resolve without treatment, most cases require antifungal medication for effective relief. According to the NHS, antifungal treatments are typically necessary to fully clear a yeast infection and prevent recurrence.
Does yeast always indicate a yeast infection?
Yeast is a normal part of the body’s microbial environment, including in the vagina. Having yeast present does not necessarily mean one has a yeast infection. A proper diagnosis is based on the presence of symptoms and an examination by a healthcare provider, not just the presence of yeast.
Do over-the-counter (OTC) vaginal care products cure yeast infections?
Over-the-counter vaginal douches and intimate care products are not effective treatments for yeast infections and can sometimes worsen the condition by disrupting the natural balance of bacteria. However, OTC antifungal treatments like miconazole can be effective for treating yeast infections, provided there is a correct diagnosis.
Is a yeast infection a sexually transmitted infection (STI)?
A yeast infection is not classified as a sexually transmitted infection (STI). However, it is possible for yeast to be transferred between partners through sexual contact if enough yeast is introduced into the vagina. Yeast infections are caused by an imbalance of yeast and do not necessarily indicate an STI.
What does vaginal yeast infection discharge look like?
Vaginal yeast infection discharge is typically thick, white, and clumpy, resembling cottage cheese. Unlike other infections, such as bacterial vaginosis, the discharge usually does not have a strong odor. Some women may experience a mild yeasty smell, but it is not overpowering. Along with discharge, symptoms like itching, irritation, and redness may also occur.
Can vaginal dryness cause a yeast infection?
Vaginal dryness itself does not directly cause yeast infections, but it can contribute to the conditions that make yeast infections more likely. Dryness can disrupt the natural balance of bacteria and yeast in the vagina, leading to irritation and increasing the risk of infection. Using lubricants or moisturizing creams can help maintain a balanced vaginal environment, especially during menopause or other hormonal changes.
Can COVID-19 lead to a vaginal yeast infection?
While there is no direct link between COVID-19 and yeast infections, some women have reported experiencing vaginal yeast infections after contracting COVID-19. This could be due to a weakened immune system, changes in the body’s stress response, or the use of antibiotics or steroids to treat COVID-19 symptoms, which can disrupt the natural balance of bacteria and yeast in the body.
Is it safe to have a vaginal yeast infection while breastfeeding?
Yes, it is generally safe to have a yeast infection while breastfeeding, but it’s important to treat it promptly. If left untreated, the infection can spread to your nipples and cause thrush, which can be painful for both mother and baby during breastfeeding. Over-the-counter antifungal creams are usually effective, but consult your doctor to ensure the treatment is safe for both you and your baby.
How effective are vaginal yeast infection creams?
Vaginal yeast infection creams are highly effective at treating yeast infections when used as directed. These antifungal creams work by targeting the yeast overgrowth in the vagina, reducing symptoms such as itching, burning, and discharge. Depending on the severity of the infection, treatment can last anywhere from 1 to 7 days. Some creams are available over-the-counter, while others require a prescription from your doctor.
Conclusion
Vaginal yeast infections are a common and manageable health concern for many women. By understanding the symptoms, causes, and treatment options, women can take proactive steps to address and prevent these infections. Open communication with healthcare providers and timely treatment are key to managing and alleviating the discomfort associated with yeast infections.