Premenstrual Syndrome (PMS) Symptoms, Causes and Treatments
What Is Premenstrual Syndrome, PMS ?
Premenstrual syndrome, often referred to as PMS, is a condition that affects many women during their childbearing years. It’s a collection of physical and emotional symptoms that typically start to surface a few days to two weeks before menstruation. While PMS is quite common, affecting up to 75 percent of women, it can vary in severity and duration from person to person. PMS can be a challenging and often uncomfortable experience, affecting various aspects of a woman’s life.
When Does PMS Typically Start ?
PMS symptoms can appear at any time between puberty and menopause. However, they most commonly start to become problematic in the late 20s to early 30s. It’s important to note that the symptoms of PMS may worsen with age and stress. Even women who have undergone hysterectomies can experience PMS if at least one functional ovary remains. Additionally, there may be a hereditary component to PMS, as women with family members who suffer from PMS are more likely to experience it themselves.
Premenstrual Syndrome, PMS Symptoms
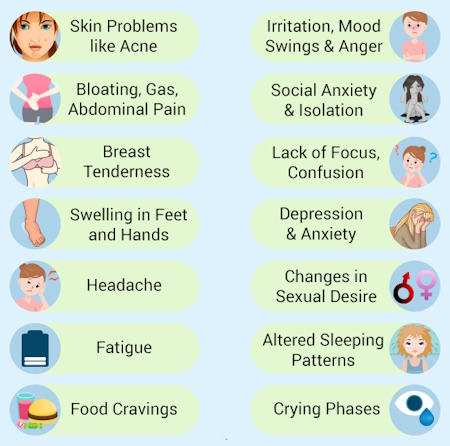
PMS encompasses a wide range of symptoms, with some women experiencing more than others. While over 150 physical and behavioral symptoms have been associated with PMS, the most commonly reported ones include:
- Irritability Feeling easily agitated or annoyed.
- Bloating A sensation of fullness or swelling in the abdominal area.
- Mood Swings Rapid and extreme shifts in emotional states.
- Anxiety Feeling anxious or worried without a clear reason.
- Depressed Mood Experiencing feelings of sadness or hopelessness.
- Fatigue A sense of tiredness or low energy.
- Appetite Changes Unusual cravings or alterations in eating habits.
- Water Retention Accumulation of fluids, often leading to swelling in the hands and feet.
- Breast Tenderness Soreness or discomfort in the breast area.
It’s important to note that menstrual cramps, although commonly associated with PMS, are not considered a PMS symptom.
Premenstrual Syndrome (PMS) Causes
The precise causes of PMS are not fully understood, but it is believed to be related to hormonal fluctuations, particularly changes in estrogen and progesterone levels during the menstrual cycle. These hormonal shifts may influence brain chemicals, including serotonin, which plays a significant role in mood regulation. Some women appear to be more sensitive to these hormone variations than others, which may explain why they develop PMS symptoms.
Diagnosing PMS
Diagnosing PMS can be challenging because there is no specific laboratory test for it. Instead, healthcare professionals rely on a pattern of symptoms that typically includes:
- Symptoms that worsen as the menstrual cycle progresses.
- Improvement in symptoms within a few days of menstruation.
- The presence of symptoms for at least two to three consecutive menstrual cycles.
To aid in diagnosis, keeping a menstrual cycle diary or checklist to track your symptoms and their severity can be immensely helpful. Additionally, your healthcare provider may inquire about your personal and family medical history and perform a physical examination. While laboratory tests are not routine for diagnosing PMS, they may be used to rule out other conditions with similar symptoms.
Keep a record of your symptoms for at least three consecutive months. This helps you and your healthcare provider identify any patterns that may suggest PMS.
Record the date when, and if, any of the following symptoms occur over two to three consecutive months, noting their severity (e.g., 1 = mild, 2 = moderate, 3 = severe). Different diaries may use varying rating systems, with point values for severity ranging from 1 to 6.
Physical Symptoms
- Abdominal bloating
- Breast tenderness
- Constipation
- Diarrhea
- Dizziness
- Fatigue
- Headache
- Swelling of hands/feet
Emotional Symptoms
- Anger
- Anxiety
- Depressed mood
- Irritability
- Mood swings
- Tension
Behavioral Symptoms
- Crying spells and tearfulness
- Decreased or increased appetite
- Difficulty concentrating
- Difficulty sleeping
- Forgetfulness
- Hostility
In addition to recommending a menstrual cycle diary, your healthcare provider will likely inquire about your personal and family medical history and perform a physical examination.
While routine laboratory tests are not standard, they may be conducted to rule out other conditions with similar symptoms, such as hypoglycemia, mania, depression, thyroid disorders, anemia, endometriosis, allergies, fibroids, dysmenorrhea, lupus, endocrine abnormalities, neurological problems like brain tumors, and heart issues.
Since menopause and PMS share some symptoms, your healthcare provider may consider your age and medical history. They may want to confirm whether you are indeed ovulating and experiencing PMS rather than menopausal symptoms. To do this, you might be asked to use an over-the-counter ovulation testing kit for home testing, which provides insights into likely ovulation timing.
If you are approaching menopause (average age around 51 for U.S. women but with a range of 42 to 60 years), blood hormone tests may also be used to confirm your menopausal status. However, a single blood test may not be informative, as hormone levels fluctuate frequently.
Premenstrual Dysphoric Disorder (PMDD)
While PMS is common, some women experience a more severe form known as Premenstrual Dysphoric Disorder (PMDD). PMDD shares many of the same symptoms as PMS but is characterized by more intense mood-related symptoms and greater disruption to daily life. To receive a PMDD diagnosis, the symptoms must be severe enough to significantly impair a woman’s daily functioning.
PMDD may be treated with serotonergic antidepressant medications or specific brands of birth control pills. It’s essential to discuss treatment options with your healthcare provider and carefully weigh the potential risks and benefits.
Premenstrual Syndrome (PMS) Treatment
Coping with PMS can be challenging, but there are various strategies and treatments available to help alleviate its discomfort. Here are some approaches to managing PMS:
Tracking Symptoms Keeping a menstrual cycle diary or symptom chart can help you identify patterns in your symptoms and develop effective strategies for managing them.
Dietary Changes Modifying your diet can have a significant impact on PMS symptoms. Increasing calcium intake, reducing refined sugar consumption, limiting caffeine and nicotine, decreasing alcohol intake, lowering salt intake, and staying hydrated are all dietary changes that may help.
Exercise Regular physical activity, such as brisk walking, jogging, biking, or swimming, can help relieve and possibly prevent PMS symptoms. Aim for at least 30 minutes of exercise on most days.
Calcium Supplements Taking calcium supplements (around 1,000 to 1,200 mg daily) may help alleviate PMS symptoms. Calcium can be found in various foods, including dairy products, tofu, broccoli, and certain fish.
Medication In cases of severe PMS, your healthcare provider may recommend medication. This can include nonsteroidal anti-inflammatory drugs (NSAIDs) for pain relief. If diet, exercise, and calcium supplements do not sufficiently alleviate mood swings or emotional PMS symptoms, consider discussing serotonin reuptake inhibitor (SSRI) antidepressants with your healthcare professional. Other prescription medications for severe PMS include gonadotropin-releasing hormone (GnRH) agonists and oral contraceptives. Some oral contraceptives, such as those containing drospirenone and ethinyl estradiol, are FDA-approved for treating emotional and physical PMDD symptoms. However, these contraceptives should only be used for PMDD if chosen for birth control, as other treatments pose fewer risks.
Preventing Premenstrual Syndrome (PMS)
While PMS cannot always be entirely prevented, many women find relief from their symptoms by adopting certain lifestyle changes and strategies.
Lifestyle Changes for PMS
Lifestyle adjustments recommended for treating PMS may also be helpful in preventing symptoms. Engage in aerobic activities like brisk walking, jogging, biking, or swimming for at least two hours and 30 minutes per week of moderate-intensity exercise or one hour and 15 minutes of vigorous-intensity exercise. Strengthen your muscles through exercise at least twice a week. Some women benefit from a balanced diet, with an emphasis on whole grains, vegetables, fruits, and reduced salt, sugar, alcohol, and caffeine intake. Maintain consistent sleep patterns and establish a bedtime routine to promote quality sleep. Stress management and sufficient rest are crucial, as sleep requirements may vary during the menstrual cycle. stress-reduction techniques such as mindfulness, meditation, or yoga to help manage emotional symptoms.
Diet for PMS Relief
To reduce PMS symptoms, spread your daily caloric intake over three small meals and three snacks, avoiding prolonged periods without eating. Gradually decrease caffeine intake, which can worsen breast tenderness and headaches. Lowering salt intake can alleviate fluid retention. Consider snacks like plain yogurt, unsalted nuts, seeds, popcorn , whole-wheat bread with peanut butter, pumpkin or banana bread, graham crackers, unsalted whole-grain crackers, bran or oatmeal muffins, raw vegetables, and raw or dried fruits.
Calcium for PMS Alleviation
If you experience physical and psychological PMS symptoms, calcium may provide relief. In one study, women who took 600 mg of calcium twice daily experienced fewer PMS symptoms compared to those taking a placebo. You can obtain calcium through your diet or calcium supplements, but consult your healthcare professional before starting supplements.
Menstrual Cycle Diary
Keep a PMS symptom diary to track when symptoms occur, their severity, and any patterns that emerge.
Frequently Asked Questions (FAQs)
What is the difference between PMS and PMDD, and how are they treated?
Premenstrual Syndrome (PMS) and Premenstrual Dysphoric Disorder (PMDD) share similar symptoms, but PMDD is a more severe form of PMS with extreme mood changes and emotional distress. Treatment for PMS and PMDD can range from lifestyle modifications and over-the-counter medications to antidepressants, hormonal treatments, and cognitive-behavioral therapy. PMDD may require more specialized medical attention due to its significant impact on daily life.
When does premenstrual syndrome (PMS) start?
PMS typically starts about 1-2 weeks before the onset of menstruation, during the luteal phase of the menstrual cycle. Symptoms may vary in intensity and duration from one cycle to the next, but they generally resolve once the period begins or shortly afterward.
How long can PMS last?
PMS symptoms usually last for about 5-10 days before menstruation and disappear once the menstrual flow starts. In some cases, symptoms may continue for a few days into the period. The duration of PMS can vary from person to person.
What are the differences between premenstrual syndrome (PMS) and pregnancy symptoms?
Premenstrual syndrome (PMS) and early pregnancy symptoms can often be similar, making it hard to distinguish between the two. PMS symptoms such as breast tenderness, fatigue, and mood swings are also common in early pregnancy. However, pregnancy-specific symptoms may include missed periods, nausea (morning sickness), and food cravings. If in doubt, a pregnancy test is recommended to confirm pregnancy.
What is considered severe premenstrual syndrome (PMS)?
Severe PMS occurs when the symptoms significantly interfere with daily life, work, and relationships. This may include intense mood swings, severe fatigue, and physical pain. In some cases, severe PMS could indicate PMDD, which requires medical evaluation and treatment.
What are some effective self-care tips for managing premenstrual syndrome (PMS)?
Self-care for PMS can include regular physical activity, a balanced diet rich in whole grains, fruits, and vegetables, and stress reduction techniques such as yoga, meditation, or deep breathing exercises. Staying hydrated and avoiding caffeine, alcohol, and salty foods can also help alleviate symptoms. Additionally, getting adequate sleep and rest is crucial for managing PMS symptoms.
Are there supplements that can help alleviate premenstrual syndrome (PMS) symptoms?
Yes, certain supplements are known to help reduce PMS symptoms. These include calcium, magnesium, vitamin B6, and vitamin D. Omega-3 fatty acids and evening primrose oil are also believed to support hormonal balance. However, it is essential to consult with a healthcare provider before starting any supplements to ensure they are appropriate for your needs.
Can PMS cause nausea?
Yes, premenstrual syndrome (PMS) can cause nausea in some individuals. This symptom may occur due to hormonal fluctuations, particularly changes in progesterone levels, during the luteal phase of the menstrual cycle.
Does PMS lead to fatigue?
Fatigue is a common symptom of PMS, and it often occurs due to hormonal changes, particularly the drop in estrogen and progesterone levels leading up to menstruation. This fatigue can make it difficult to concentrate and perform daily tasks.
Is breast pain normal during premenstrual syndrome (PMS)?
Yes, breast pain or tenderness is a common symptom of PMS. It occurs due to hormonal changes that cause fluid retention and swelling in the breast tissue. This symptom usually resolves once menstruation begins.
Can PMS symptoms mimic a heart attack?
In rare cases, severe PMS symptoms such as chest pain, shortness of breath, and anxiety may mimic the symptoms of a heart attack. However, these symptoms are more likely caused by hormonal changes and stress. If you experience chest pain or other symptoms associated with a heart attack, seek medical attention immediately to rule out any serious conditions.
Conclusion
Premenstrual Syndrome (PMS) is a common condition that affects many women of childbearing age. While it can be uncomfortable and disruptive, various strategies and treatments are available to manage its symptoms. By making dietary changes, engaging in regular exercise, and considering medical interventions when necessary, women can find relief and improve their quality of life. Additionally, tracking symptoms and adopting preventive measures can help reduce the impact of PMS. If you suspect you have PMS or are struggling with its effects, consult with a healthcare professional for guidance and support. Remember that you don’t have to face PMS alone, and there are effective ways to address its challenges.










