Placental Abnormalities: Types, Complications, and Management
The placenta is a crucial organ that forms during pregnancy, serving as the lifeline between the mother and the developing fetus. It facilitates the transfer of nutrients and oxygen while also eliminating waste products from the fetus. Any abnormalities in the placenta can pose significant risks to both maternal and fetal health, leading to complications during pregnancy and delivery.
What Are Placental Abnormalities?
Placental abnormalities refer to conditions where the placenta does not develop or function properly during pregnancy. Anomalies can arise during any stage of placental development, impacting the organ’s structure and function. Normally, the placenta attaches to the upper part of the uterus, but abnormal positioning or structural issues can lead to complications that may affect pregnancy outcomes. The placenta’s roles include nutrient and oxygen transfer to the fetus, hormone production, and waste removal, all of which are crucial for fetal health. Disruptions in these functions can have far-reaching consequences.
Types of Placental Abnormalities
Several types of placental abnormalities can occur during pregnancy. Understanding these types is essential for anticipating potential complications and determining appropriate management strategies. Below are some common placental abnormalities:
1. Placenta Previa
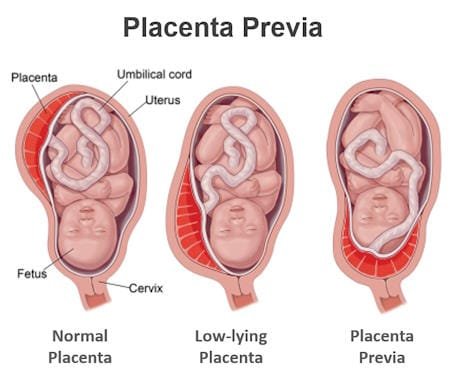
Placenta previa is a condition where the placenta implants in the lower segment of the uterus, covering part or all of the cervix. This condition is classified into different types:
- Complete Previa: The internal cervical os is completely covered by the placenta, which poses a significant risk during delivery.
- Partial Previa: The placenta partially covers the internal os, potentially leading to complications.
- Marginal Previa: The edge of the placenta extends to the edge of the cervical os, increasing the risk of bleeding.
- Low-Lying Placenta: The placenta is positioned within 2 cm of the cervical os without covering it.
Placenta previa is a significant cause of third-trimester bleeding and can lead to severe maternal morbidity, including hemorrhage requiring transfusion, disseminated intravascular coagulation, and emergency hysterectomy. Symptoms often include bright red vaginal bleeding without pain during the third trimester. Diagnosis is typically made via ultrasound, and treatment options may include bed rest, avoiding sexual activity, and cesarean delivery in severe cases. Regular monitoring through ultrasound can help track the position of the placenta and guide clinical decision-making.
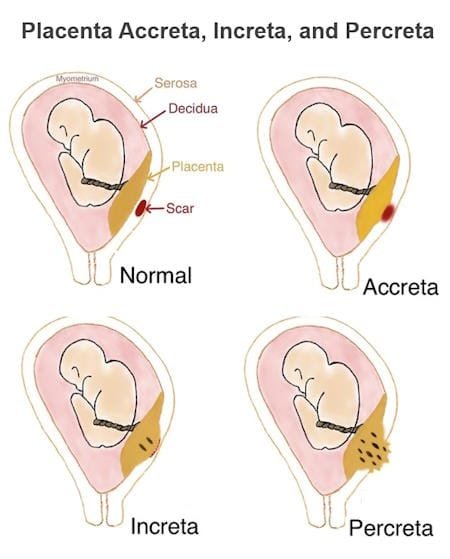
2. Placenta Accreta, Increta, and Percreta
Placenta accreta is characterized by abnormal adherence of the placenta to the uterine wall, often due to previous cesarean deliveries or uterine surgeries. This abnormality can lead to several complications, including:
- Placenta Increta: In this condition, the placental villi penetrate the uterine muscle but do not breach the uterine outer lining, leading to potential complications during delivery.
- Placenta Percreta: The placental villi invade through the uterine muscle to the uterine outer lining and even invade the nearby blood vessels and organs like urinary bladder , which can result in severe hemorrhage and necessitate surgical intervention.
These conditions can result in severe complications, including postpartum hemorrhage, the need for hysterectomy, massive blood transfusion and in extreme cases, maternal mortality. Ultrasound findings, such as the absence of a clear area behind the placenta and uterine muscle thinning, can aid in diagnosing these conditions. An MRI can further enhance diagnostic accuracy, especially in high-risk cases.
3. Vasa Previa
Vasa previa occurs when fetal blood vessels run between the baby and the cervix, making them susceptible to rupture during labor. This condition often presents with painless vaginal bleeding in the second or third trimester, which can pose severe risks to the fetus. Early detection through ultrasound is essential, as timely cesarean delivery can prevent severe fetal blood loss. Management strategies typically involve careful monitoring and scheduling an elective cesarean delivery around 35 weeks of gestation to minimize risks. Awareness of this condition is crucial, especially in pregnancies complicated by abnormal placentation.
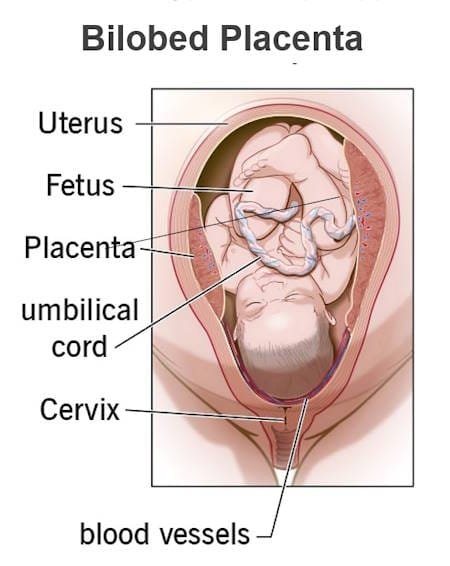
4. Bilobed and Succenturiate Placenta
A bilobed placenta consists of two roughly equal-sized lobes connected by membranes and occurs in about 2% to 8% of placentas. While it is not usually associated with increased fetal anomalies, it can lead to complications such as first-trimester bleeding and placental abruption. In some cases, there may also be issues related to the distribution of blood vessels, which can affect fetal growth.
A succenturiate placenta has one or more smaller accessory lobes that are not part of the main placental body. This condition can lead to complications such as retained placenta after delivery, which can cause severe hemorrhage, and vasa previa if fetal vessels connect to the succenturiate lobe.
5. Circumvallate and Circummarginate Placenta
Circumvallate placenta features a ring-like structure formed by a double fold of chorion, leading to various complications, including premature rupture of membranes, preterm delivery, and possible fetal growth restriction. In some cases, the presence of a circumvallate placenta may be associated with higher risks of adverse outcomes such as intrauterine growth restriction and placental abruption.
Circummarginate placenta is similar but has a flat transition from the membranous to villous chorion, which is typically clinically insignificant. However, it is essential for healthcare providers to monitor pregnancies with circumvallate placentas closely, as complications can arise unexpectedly.
6. Other Rare Placental Abnormalities
Additional placental abnormalities include:
- Placenta Membranacea: A condition where chorionic villi cover the fetal membranes, which can lead to complications such as placenta accreta and poor fetal outcomes.
- Ring-Shaped Placenta: An annular-shaped placenta that can cause bleeding and fetal growth restriction due to compromised blood supply.
- Placenta Fenestrata: A rare defect characterized by missing central portions of the placenta, which may lead to functional impairments.
- Battledore Placenta: Occurs when the umbilical cord is inserted at or near the placental margin, increasing the risk of complications such as intrauterine growth restriction, cord accidents, and even placental abruption.
Complications Associated with Placental Abnormalities
Placental abnormalities can lead to several complications that affect both maternal and fetal health, including:
- Hemorrhage: Severe bleeding can occur during pregnancy and delivery, which may lead to life-threatening conditions for both the mother and child. In cases of placenta previa, the risk of hemorrhage increases significantly, especially during labor.
- Preterm Birth: Abnormalities such as placenta previa or abruption can increase the risk of premature delivery, which can have long-term effects on the child’s health, including developmental delays and respiratory issues.
- Fetal Growth Restriction: Insufficient blood flow and nutrients to the fetus can impede proper growth and development, leading to low birth weight and other complications.
- Emergency Hysterectomy: In cases of severe placenta accreta or previa, a hysterectomy may be necessary to save the mother’s life, especially in the presence of uncontrollable hemorrhage.
- Intrauterine Fetal Death: Severe placental complications may lead to fetal demise in utero, particularly in cases of vasa previa or severe growth restriction.
- Maternal Morbidity: Complications associated with placental abnormalities can lead to increased rates of maternal morbidity, including infection, prolonged hospitalization, and long-term health issues.
Management of Placental Abnormalities
The management of placental abnormalities depends on the type and severity of the condition. Healthcare providers must consider the risks associated with each abnormality while developing a comprehensive management plan. Common approaches include:
- Monitoring: Regular ultrasounds and check-ups to monitor the placenta’s position and functionality. For conditions like placenta previa, healthcare providers may schedule more frequent appointments to assess any changes in the placenta’s position.
- Bed Rest: For conditions like placenta previa, doctors may recommend bed rest to minimize the risk of bleeding and complications. Patients are often advised to avoid strenuous activities and sexual intercourse.
- Medications: In some cases, medications may be prescribed to manage symptoms and reduce complications. For instance, tocolytics may be used to prevent preterm labor in patients with certain placental issues.
- Surgical Interventions: Cesarean delivery is often the preferred method for placental abnormalities that pose a risk during vaginal delivery. In cases of severe placenta accreta, a multidisciplinary team may be required to manage the delivery and any necessary surgical interventions.
- Blood Transfusions: In cases of severe bleeding, blood transfusions may be necessary to stabilize the mother and prevent shock.
- Education and Counseling: Providing education to expectant mothers about their condition and potential complications is crucial. Counseling can help them understand the risks and the need for careful monitoring and management.
Frequently Asked Questions (FAQs)
What are the symptoms of an abnormal placenta during pregnancy?
Symptoms may vary depending on the specific abnormality but can include painless vaginal bleeding, severe abdominal pain, or signs of preterm labor. It is crucial to report any unusual symptoms to a healthcare provider promptly. Early recognition of symptoms associated with placental abnormalities can significantly improve outcomes for both mother and baby.
Is a bilobed placenta dangerous?
A bilobed placenta is not typically associated with severe risks for the fetus; however, it can lead to complications such as first-trimester bleeding and placental abruption. Regular monitoring and communication with healthcare providers are essential for managing this condition effectively. Patients should be aware of the potential risks associated with their specific type of placental abnormality and discuss them with their healthcare provider.
What are the risks of a bilobed placenta?
While a bilobed placenta itself may not pose significant risks, it can be associated with other complications, such as polyhydramnios (excess amniotic fluid), placental abruption, and first-trimester bleeding. Careful monitoring is important to ensure both maternal and fetal health. The presence of a bilobed placenta may require additional ultrasounds to monitor fetal growth and development closely.
Can a woman have a normal delivery with a bilobed placenta?
Many women with a bilobed placenta can have a normal delivery. However, the mode of delivery will depend on the overall health of the mother and fetus, as well as any complications that may arise during pregnancy. The healthcare team will assess factors such as the baby’s position, fetal heart rate, and overall maternal health before deciding on the best delivery method.
How can placental abnormalities be diagnosed?
Placental abnormalities are typically diagnosed through ultrasound imaging, which can provide valuable information about the placenta’s location, structure, and any potential issues. Healthcare providers may also use Doppler ultrasound to assess blood flow and identify any abnormalities in fetal vessels. In certain cases, MRI may be utilized for more detailed imaging, especially when complications are suspected.
What is the treatment for placenta previa?
The treatment for placenta previa depends on the degree of placental coverage of the cervix, the presence of bleeding, and the gestational age. If a woman is diagnosed with placenta previa and is not experiencing bleeding, she may be monitored with regular ultrasounds to assess the placenta’s position. In cases where there is significant bleeding or if the placenta is covering the cervix late in pregnancy, cesarean delivery is typically recommended.
Are there any long-term effects of placental abnormalities?
While many women with placental abnormalities can have healthy pregnancies and deliveries, there can be long-term effects depending on the severity of the condition and any complications that arise. For instance, women who experience significant hemorrhage during delivery may face risks of anemia or require future surgical interventions. Additionally, babies born to mothers with placental abnormalities may be at higher risk for certain health issues, such as low birth weight and developmental delays, which require ongoing monitoring and support.
Conclusion
Understanding placental abnormalities is essential for expecting mothers and healthcare providers alike. These conditions can significantly impact pregnancy outcomes, and early detection is key to managing potential complications. Regular prenatal care, including ultrasounds and health assessments, can help identify placental issues early and enable timely interventions. If you have concerns about placental abnormalities, do not hesitate to consult with your healthcare provider for personalized advice and management strategies.