Mycoplasma Genitalium (Mgen): Symptoms, Causes & Treatment
Mycoplasma genitalium (commonly referred to as Mgen or M. genitalium) is a sexually transmitted infection (STI) caused by a microscopic bacterium. This infection spreads through sexual contact with an infected individual and is particularly prevalent among young people and those who do not consistently use condoms during sexual activity.
Although often asymptomatic, Mycoplasma genitalium can lead to serious health complications if left untreated. Alarmingly, there is growing concern about Mgen’s potential to evolve into a ‘superbug’—a bacterium resistant to current antibiotic treatments.
Although less well-known than other STIs like syphilis and gonorrhea, Mycoplasma genitalium is increasingly recognized as a growing concern, and early detection and appropriate treatment are essential to managing its impact.
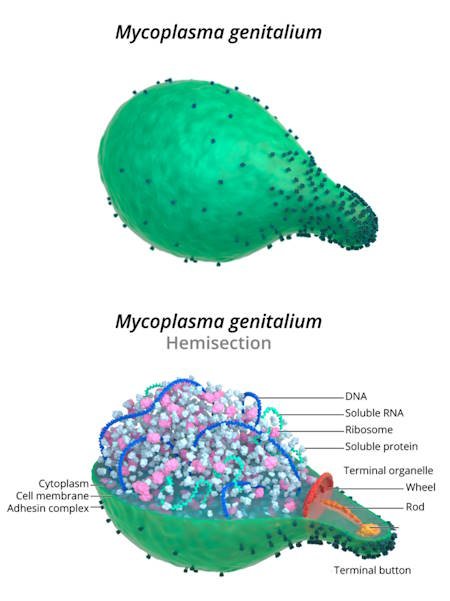
What Is Mycoplasma Genitalium?
Mycoplasma genitalium is a relatively newly recognized STI, first identified in 1981. For years, its transmission pathway was unclear, and diagnostic tests were unavailable. Reliable testing for Mgen only became widely accessible in 2017, allowing for better identification and treatment of this infection.
This infection is caused by a tiny bacterium that targets the urogenital tract, impacting areas like the vagina, uterus (womb), and Fallopian tubes in women, and the urethra and epididymis (sperm-carrying tubes) in men.
How Common Is Mycoplasma Genitalium?
In the United States, Mycoplasma genitalium (Mgen) has experienced the most significant increase in medical insurance claims for any STD. Originally identified in the early 1980s, this bacterium has seen a staggering 197% surge in infection rates from 2007 to 2018.
Other data reveals that the number of new *Mycoplasma genitalium* infections has nearly tripled in both urban and rural areas, highlighting the widespread nature of this increase.
As a result of these troubling statistics, health organizations such as the Centers for Disease Control and Prevention (CDC) have issued special warnings. The bacterium has now been included in the list of top three pathogens that require heightened monitoring. Another reason for its increased scrutiny is the growing concern over its potential to become more antibiotic-resistant, as recent research points to this troubling trend.
In the U.S., studies estimate the prevalence of *Mycoplasma genitalium* to be between 1% and 2% of the adult population. Rates are particularly high among youth under 18 years and vary by region.
Globally, estimates suggest it affects around 2% of Europeans and up to 3% of the population worldwide. Studies have found higher infection rates among individuals with multiple sexual partners, those who do not practice safe sex, smokers, and people of Afro-Caribbean ethnicity. In the United States, the infection is most prevalent among African-Americans, followed by white and Hispanic populations.
Mycoplasma Genitalium Symptoms
Most people with Mycoplasma genitalium infection do not experience symptoms. Studies suggest that 70–80% of infected men and 50–70% of infected women remain asymptomatic. However, Mgen is a common cause of nongonococcal urethritis (NGU) in men and pelvic inflammatory disease (PID) in women.
When symptoms occur, they typically appear 1–3 weeks after infection and may include the following:
Symptoms of Mycoplasma Genitalium in Men
- Urethritis (swelling and inflammation of the urethra).
- Painful urination.
- Discomfort during ejaculation.
- Watery or cloudy discharge from the penis.
- Inflammation of the rectum (proctitis).
- Swelling of the foreskin or penis.
Symptoms of Mycoplasma Genitalium in Women
- Urethritis, leading to pain during urination and external genital soreness.
- Increased or unusual vaginal discharge.
- Bleeding between periods.
- Cervicitis (inflammation of the cervix), causing pain during intercourse or post-intercourse bleeding.
- Lower abdominal pain.
How Does Mycoplasma Genitalium Differ from Chlamydia?
While the symptoms of Mycoplasma genitalium closely resemble those of chlamydia, the two infections are caused by different bacteria. Historically, many cases of Mgen were misdiagnosed as chlamydia, potentially contributing to antibiotic resistance in Mgen due to inappropriate treatment. Notably, it is possible to have both infections simultaneously, although Mgen is less prevalent and slightly harder to transmit than chlamydia.
For more details on chlamydia, refer to our separate article on Chlamydia.
How Is Mycoplasma Genitalium Transmitted?
Mycoplasma genitalium spreads through sexual contact with an infected individual. It is primarily transmitted through genital-to-genital contact, including vaginal or anal sex, and may occur even without penetration.
Can Mycoplasma Genitalium Be Transmitted Through Oral Sex?
While the exact likelihood of transmission through oral sex is unclear, it is considered possible.
Do Condoms Protect Against Mycoplasma Genitalium?
Yes, condoms provide a high level of protection against Mycoplasma genitalium. Although not 100% effective, both male and female condoms significantly reduce direct genital tissue contact, minimizing the risk of transmission.
Complications of Mycoplasma Genitalium Infection
The complications of Mycoplasma genitalium infection arise mainly due to the immune system’s reaction to the bacterium. However, the bacterium itself can also damage the Fallopian tube lining, leading to serious reproductive health issues. These complications are similar to those caused by chlamydia and include:
Pelvic Inflammatory Disease (PID)
Pelvic Inflammatory Disease (PID) involves infection and inflammation of the uterus and Fallopian tubes. Symptoms include:
- Abdominal pain.
- Pain during intercourse.
- Fever or elevated body temperature.
- General unwellness.
In severe cases, infection can scar and block the Fallopian tubes, potentially leading to tubal infertility.
Sexually Acquired Reactive Arthritis (SARA)
This condition occurs as a reaction to urethritis in both men and women, causing joint inflammation and discomfort.
Epididymo-Orchitis in Men
This refers to painful swelling and infection of the testicle (testis) and epididymis (the sperm-carrying tube). While not definitively proven, some studies suggest a potential link between Mgen and male infertility.
Increased Risk of Transmitting Other STIs
Individuals with both Mgen and other STIs, such as HIV, may have an elevated risk of transmitting these infections to their partners.
Mycoplasma Genitalium and Pregnancy
Mycoplasma genitalium has been linked to complications such as preterm birth and miscarriage. It is possible that Mgen can be transmitted to the baby during vaginal delivery, though it remains unclear whether it can be passed to the baby in the womb or if this would cause harm.
If diagnosed with Mycoplasma genitalium during pregnancy, it is crucial to inform your healthcare provider. Not all antibiotics used to treat Mgen are safe during pregnancy, so tailored treatment is essential.
Testing for Mycoplasma Genitalium
Mycoplasma genitalium is detected through specialized laboratory tests. These tests typically involve vaginal swabs for women or ‘first void’ urine samples for men. Since the bacterium is challenging to detect, nucleic acid amplification tests (NAATs) are commonly used. Additionally, laboratories often test for antibiotic resistance to guide treatment decisions.
Who Should Be Tested?
Testing for Mycoplasma genitalium is recommended for:
- Individuals with symptoms suggestive of Mgen.
- Men diagnosed with non-gonococcal urethritis (NGU).
- Women diagnosed with pelvic inflammatory disease (PID).
- Current sexual partners of individuals diagnosed with Mgen.
Sexual partners who test positive but exhibit no symptoms should still be treated. While the impact on asymptomatic individuals remains uncertain, treatment helps prevent reinfection or transmission to others.
Can I Get Tested for Mycoplasma Genitalium?
Routine testing for Mycoplasma genitalium is not currently recommended for everyone. Testing the general population would require substantial resources and is not considered cost-effective since only 1–3% of individuals are likely to test positive. Instead, testing focuses on:
- Individuals with symptoms suggestive of Mgen.
- Patients diagnosed with pelvic inflammatory disease (PID).
- Men with non-gonococcal urethritis (NGU).
Additionally, widespread testing and treatment could accelerate antibiotic resistance, reducing the effectiveness of current therapies.
Mycoplasma Genitalium Treatment
Treating Mycoplasma genitalium has become more challenging due to the bacterium’s growing resistance to standard antibiotics. While single-dose azithromycin was once the mainstay treatment, longer and more complex regimens are now necessary.
Current Recommended Treatments
- Doxycycline: 100 mg twice daily for seven days.
- Azithromycin: 1 g as a single dose, followed by 500 mg daily for two additional days.
- Moxifloxacin: 400 mg daily for 10 days. This is reserved for cases resistant to azithromycin, though resistance to moxifloxacin is increasingly problematic in Asia.
Alternative Treatments
For cases where standard regimens are ineffective, alternative options include:
- Doxycycline 100 mg twice daily for seven days, followed by pristinamycin 1 g four times daily for 10 days.
- Pristinamycin 1 g four times daily for 10 days.
- Doxycycline 100 mg twice daily for 14 days.
- Minocycline 100 mg twice daily for 14 days.
Special Cases
In instances of pelvic inflammatory disease or epididymo-orchitis, a 14-day course of moxifloxacin (400 mg daily) is recommended.
Follow-Up Testing
A repeat test is essential three weeks after completing treatment to ensure the infection is fully eradicated. Partial treatment increases the risk of antibiotic resistance, as surviving bacteria are more likely to develop resistance mechanisms.
Does Mycoplasma Genitalium Go Away By Itself?
It is highly unlikely that Mycoplasma genitalium will resolve on its own. Unlike some bacteria that the immune system can effectively eliminate, Mycoplasma genitalium is particularly resilient. These organisms can infect without causing noticeable symptoms and hide inside human cells, making it difficult for the immune system to eradicate them.
Prognosis for Mycoplasma Genitalium?
If treated successfully with antibiotics, Mycoplasma genitalium does not typically cause long-term health issues. However, untreated or advanced infections can lead to complications:
- Tubal Infertility: If pelvic inflammatory disease causes tubal damage, it can result in irreversible infertility in women.
- Potential Male Infertility: Research is ongoing regarding the impact of Mgen on male infertility, particularly in cases of epididymo-orchitis.
- Reactive Arthritis: Like chlamydia, Mgen-induced arthritis typically improves with appropriate treatment, but it may take months to resolve.
Final Thoughts
The rising prevalence of Mycoplasma genitalium highlights the urgent need for increased awareness, regular screening, and responsible antibiotic use to combat this growing public health concern. As the bacterium becomes more resistant to treatment, early detection and proper medical intervention are crucial in preventing complications and reducing its spread.
Public health entities, researchers, and healthcare providers must work together to educate the population and develop effective strategies to manage this emerging STD. By staying informed and vigilant, individuals can play a vital role in protecting their health and the well-being of their communities.
Frequently Asked Questions (FAQs)
Can You Tell If Your Partner Has Mycoplasma Genitalium?
It is not possible to visually identify whether someone has Mgen. Since the infection often causes no symptoms, your partner may be unaware of their status. Testing is the only reliable way to diagnose Mycoplasma genitalium.
Can I Have Sex While Being Treated for Mycoplasma Genitalium?
No, it is crucial to abstain from sexual intercourse until both partners have completed their treatment. Women with pelvic inflammatory disease (PID) should avoid intercourse until 14 days after starting treatment or until symptoms have fully resolved—whichever is later.
How Long Have I Had Mycoplasma Genitalium?
The exact duration of an Mycoplasma genitalium infection cannot currently be determined. Doctors have no means of identifying when the infection was acquired. It is possible for individuals who develop symptoms to have had a silent infection previously. This means that a diagnosis of Mgen does not necessarily indicate a recent infection—it may have been present for some time.
Can I Get Mycoplasma Genitalium Without Having Sex?
Mgen is a sexually transmitted infection (STI) transmitted through genital-to-genital contact. It is possible to acquire the infection without full intercourse, but it requires sexually intimate contact.
Can Mycoplasma Genitalium Affect Same-Sex Relationships?
Yes, Mycoplasma genitalium can be transmitted in same-sex relationships. The infection spreads through genital-to-genital contact, including vaginal and anal contact, as well as oral-to-genital contact. The use of male or female condoms significantly reduces the risk of transmission between partners, regardless of gender.
How Can I Avoid Catching Mycoplasma Genitalium?
There are several steps to reduce the risk of contracting Mycoplasma genitalium:
- Limit the number of sexual partners.
- Consistently use condoms to reduce the likelihood of transmission.
- Quit smoking, as it has been linked to a higher risk of STIs, including Mgen.
When Can My Partner and I Stop Using Protection?
If either partner has had previous sexual partners, there is a possibility of carrying a “silent” STI such as Mycoplasma genitalium or chlamydia. To reduce risk:
- Get tested for STIs before engaging in unprotected intercourse.
- Prioritize testing if one partner has symptoms of Mgen or another STI.
- Seek medical advice if a previous partner has required treatment for an STI.
Testing and treatment are key steps to ensuring a healthy relationship free from the risk of STIs.