IUD Insertion Pain: Duration, Level, and Management
Intrauterine devices (IUDs) have become increasingly popular due to their reliability as a long-term birth control method. With effectiveness rates comparable to surgical sterilization, IUDs provide a convenient and reversible contraceptive option that doesn’t require daily maintenance. Despite these advantages, the process of IUD insertion often raises questions and concerns, particularly regarding the level of discomfort or pain involved. Addressing these concerns is crucial, as they can significantly impact a woman’s decision to choose this method of contraception.
In this blog post, we will explore various types of IUDs available, IUD insertion process, and what you can expect in terms of pain and discomfort. We’ll also cover the new CDC guidelines on pain management for IUD insertion. Additionally, we’ll evaluate the effectiveness of IUDs and provide an overview of potential side effects and risks.
By the end of this guide, you’ll have a comprehensive understanding of IUDs, equipping you to make an informed decision about whether this contraceptive method is the right choice for you.
What is an IUD?
An IUD, or intrauterine device, is a small, flexible, T-shaped contraceptive device that is inserted into the uterus through the vagina. It’s a type of long-acting, reversible contraception (LARC) that can provide birth control for three to ten years, depending on the specific type used.
IUDs work by preventing pregnancy in different ways:
- Hormonal IUDs release progestin, a synthetic version of the hormone progesterone. This causes the cervical mucus to thicken, creating a barrier that prevents sperm from reaching the egg.
- Copper IUDs don’t contain hormones. Instead, they use a small amount of copper, which triggers an immune response in the uterus. This creates an environment that’s toxic to sperm, preventing fertilization.
 Types of IUDs
Types of IUDs
There are two main categories of IUDs:
- Hormonal IUDs
- Mirena® (approved for up to 8 years)
- Liletta® (up to 8 years)
- Kyleena® (up to 5 years)
- Skyla® (up to 3 years)
- Copper IUD
- Paragard® (approved for up to 10 years)
Each type of IUD has its own set of benefits and potential side effects, which we’ll discuss in more detail later.
 IUD Insertion: What to Expect
IUD Insertion: What to Expect
The insertion process typically involves the following steps:
- Your healthcare provider will insert a speculum into your vagina, similar to a routine pelvic exam.
- They will use a small tube to pass the IUD through the cervical opening and into the uterus.
- The entire procedure usually takes only a few minutes.
Pain During IUD Insertion
One of the most common concerns women have about IUDs is the pain associated with insertion. The level of discomfort during IUD insertion can vary greatly from person to person. While some women find the procedure uncomfortable and experience intense cramping during insertion, others may continue to feel cramping afterward. However, the vast majority of patients manage the process well and find the discomfort manageable. Some factors that may influence the pain experience include:
- Whether you’ve given birth before: Women who have not been pregnant before may experience more cramping, as their uterus is smaller and the IUD may cause more irritation.
- Your typical menstrual cramps: If you usually experience intense cramping during your period, you may be more likely to have stronger cramps during and after IUD insertion.
- Overall pain tolerance and anxiety levels: Research suggests that pain perception can be influenced by anxiety and fear of pain itself.
- Type of IUD: Some women report differences in pain levels between hormonal and copper IUDs, though this can vary.
It’s important to note that while the insertion process may be uncomfortable, it is typically brief. Many women find that the benefits of long-term, highly effective contraception outweigh the short-term discomfort of insertion.
New CDC Guidelines on Pain Management for IUD Insertion
The Centers for Disease Control and Prevention (CDC) has recently updated its recommendations for healthcare providers regarding pain management during IUD insertion. These new guidelines aim to address patient concerns and improve the overall experience of getting an IUD. Key points from the updated CDC recommendations include:
- Emphasis on patient-centered care: The CDC encourages healthcare providers to develop personalized pain management plans based on individual patient preferences.
- Lidocaine as a pain relief option: The use of lidocaine, a local anesthetic, is now recommended as a potentially effective method for reducing pain during IUD insertion. This can be administered as an injection (paracervical block) or applied topically as a gel, cream, or spray.
- Limitations of over-the-counter painkillers: The CDC notes that commonly suggested pain relievers like aspirin or ibuprofen have shown little evidence of effectiveness in reducing pain or improving patient satisfaction during IUD insertion.
- Misoprostol not recommended: The CDC specifically advises against the routine use of misoprostol before IUD insertion, as it may actually increase patient discomfort and cause side effects like cramping and diarrhea.
- Insurance coverage: Under federal guidelines, most private health insurance plans are required to fully cover contraceptive care, including related services such as pain management for IUD insertion. This means patients should not face additional costs for these pain relief options.
These updated recommendations come in response to growing awareness of patient experiences and concerns about pain during IUD insertion. By providing more options for pain management and encouraging open communication between patients and healthcare providers, the CDC aims to improve access to and satisfaction with this highly effective form of contraception.
It’s important for patients to discuss these pain management options with their healthcare providers when considering an IUD. Every individual’s experience is unique, and working together with your provider can help ensure the most comfortable insertion process possible.
Post IUD Insertion Experience
After the IUD is inserted, you may experience:
- Continued cramping: Some women have cramps for one to two days following insertion.
- Irregular bleeding: This is common, especially with hormonal IUDs, and typically lasts for the first three to six months.
- Spotting: With copper IUDs, you may experience some spotting after insertion or for the first couple of months.
Follow-up visits are generally not necessary unless you experience severe pain (beyond normal cramping), heavy bleeding, abnormal vaginal discharge, fever, or if you suspect the IUD has been expelled.
Choosing the Right IUD for You
When deciding which type of IUD is best for you, consider the following factors:
- Desired menstrual effects:
- Hormonal IUDs often lead to lighter periods or no periods at all.
- Copper IUDs typically allow for regular monthly periods, which may be heavier or more painful, especially in the first few months.
- Duration of effectiveness:
- Hormonal IUDs last between 3 to 8 years, depending on the brand.
- The copper IUD is effective for up to 10 years.
- Hormone sensitivity: If you’re sensitive to hormones or prefer hormone-free birth control, a copper IUD might be the better choice.
- Future pregnancy plans: All IUDs can be removed at any time if you decide to try for pregnancy.
You should discuss these factors with your healthcare provider to make an informed decision.
Effectiveness of IUDs
IUDs are one of the most effective forms of reversible contraception available. They have a typical one-year failure rate of less than 1%, making them more effective than many other birth control methods, including the pill.
Hormonal IUDs become effective within seven days of insertion, while copper IUDs work immediately after placement. It’s worth noting that both types of IUDs can be used as emergency contraception if inserted within five days of unprotected intercourse.
Potential Side Effects and Risks
While IUDs are generally safe and well-tolerated, there are some potential side effects and risks to be aware of:
- Irregular bleeding: This is common with hormonal IUDs, especially in the first few months.
- Increased menstrual bleeding and cramping: More common with copper IUDs.
- IUD expulsion: In rare cases, the IUD may come out of the uterus on its own. If this happens, you’ll need to have it replaced by a healthcare provider.
- Uterine perforation: In very rare instances, the IUD may move through the uterine wall. This would require surgical removal.
- Infection: There’s a slight risk of infection (less than 1%) within the first three to six months following insertion. If an infection occurs, it can typically be treated with antibiotics.
It’s important to remember that serious complications from IUDs are rare, and many women use them without experiencing significant side effects.
IUD Removal
You can have your IUD removed at any time, whether you’ve reached the end of its effective lifespan or you’ve decided to try for pregnancy. The removal process is generally less uncomfortable and quicker than insertion.
Usually, women just have one big cramp as it’s removed, and there isn’t any cramping afterward. In rare cases where the IUD strings are not visible, a special instrument may be needed for removal, which could feel similar to the initial insertion.
IUDs and Cancer Risk
Research suggests that all types of IUDs may reduce the risk of uterine and ovarian cancer. However, recent studies have shown a small increase in breast cancer risk among women who use or have recently used hormonal contraceptives, including combined oral contraceptives and progestin-only methods.
It’s important to note that the data regarding IUDs and breast cancer risk is not conclusive. Dr. Madden advises, “Even if a woman has a family history of breast cancer, it doesn’t always mean she can’t have an IUD. But we like to discuss the risks with our patients because we believe they should be educated.”
Women with active breast cancer should not use hormonal IUDs, and those with cervical or uterine cancer may not be candidates for any type of IUD.
Who Can Use IUDs?
Most women can safely use IUDs, but there are some exceptions:
- Women with current sexually transmitted infections (STIs) or pelvic infections
- Those who may be pregnant
- Women with a copper allergy or Wilson disease (for copper IUDs)
- In some cases, the size or shape of a woman’s uterus may make it difficult to place an IUD correctly
It’s crucial to have a thorough discussion with your healthcare provider about your medical history and any concerns before deciding on an IUD.
Conclusion
Intrauterine devices offer a highly effective, long-term contraceptive option for many women. While the insertion process may cause some discomfort, advances in pain management techniques and increased awareness among healthcare providers are making the experience more manageable for patients.
By understanding the types of IUDs available, what to expect during insertion, and potential side effects, you can make an informed decision about whether an IUD is right for you. Remember, every woman’s experience is unique, and open communication with your healthcare provider is key to finding the best contraceptive solution for your needs.
Frequently Asked Questions (FAQs)
How does IUD insertion pain compare to childbirth?
IUD insertion pain is typically much less intense than the pain experienced during childbirth. The insertion procedure may cause cramping and discomfort similar to menstrual cramps, but it is usually brief. Most women find the pain manageable, especially with pain relief options like over-the-counter painkillers.
Is it normal to experience pain after sex with an IUD?
Mild discomfort or cramping after sex with an IUD is not uncommon, especially in the first few weeks after insertion. However, persistent or severe pain may indicate that the IUD has shifted or there is another underlying issue. If you experience ongoing pain after sex, consult your healthcare provider.
Why do I experience pain during sex with an IUD?
Pain during sex with an IUD can occur if the device is improperly positioned or if it is causing irritation. Sometimes, the IUD strings might be felt by your partner, which can also lead to discomfort. If you consistently experience pain during sex, it’s important to have your IUD placement checked by a healthcare professional.
What are the options for managing IUD insertion pain?
Pain management for IUD insertion includes taking over-the-counter pain relievers like ibuprofen before the procedure. Some providers may offer a local anesthetic or recommend deep breathing exercises to help manage discomfort. If you experience severe pain during or after insertion, contact your healthcare provider.
How long does pain last after IUD insertion?
Pain and cramping after IUD insertion usually last for a few hours to a couple of days. Mild cramping and spotting can continue for a few weeks as your body adjusts to the IUD. If the pain persists beyond this period or becomes severe, you should consult your healthcare provider.
Can an IUD cause long-term pain?
While most women adjust to their IUD within a few months, some may experience ongoing discomfort or pain. This could be due to the IUD being improperly positioned, or it may simply not be the right contraceptive method for you. If long-term pain occurs, a healthcare provider can assess whether the IUD should be removed or repositioned.
What should I do if I experience severe pain after IUD insertion?
Severe pain after IUD insertion is not typical and could indicate a complication such as perforation or infection. If you experience intense pain, heavy bleeding, or signs of infection (such as fever), seek medical attention immediately.

 Types of IUDs
Types of IUDs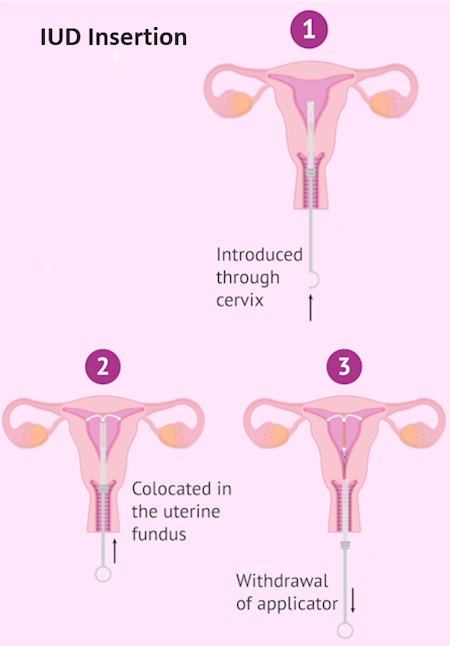 IUD Insertion: What to Expect
IUD Insertion: What to Expect







