How to Identify HIV Rash: Pictures & Treatment
Skin problems are a common occurrence among individuals living with HIV. Almost every person diagnosed with HIV will experience some form of skin issue during the course of their illness. These skin conditions can range from those that are common in the general population to those specifically associated with HIV. One of the early indicators of HIV infection is the appearance of an HIV-specific rash, which often prompts individuals to seek medical advice. For more details about HIV (Human Immunodeficiency Virus) read “HIV / AIDS: Symptoms, Diagnosis, Treatment, and Prevention”
What is an HIV Rash?
An HIV rash is a skin condition that affects approximately 90% of people living with HIV at some stage during their illness. The high prevalence of skin issues among HIV patients is primarily due to the virus’s impact on the immune system. When the immune system is compromised, the body becomes more susceptible to various infections and skin conditions. The appearance, severity, and color of the rash can vary depending on several factors, including the cause and the stage of the disease.
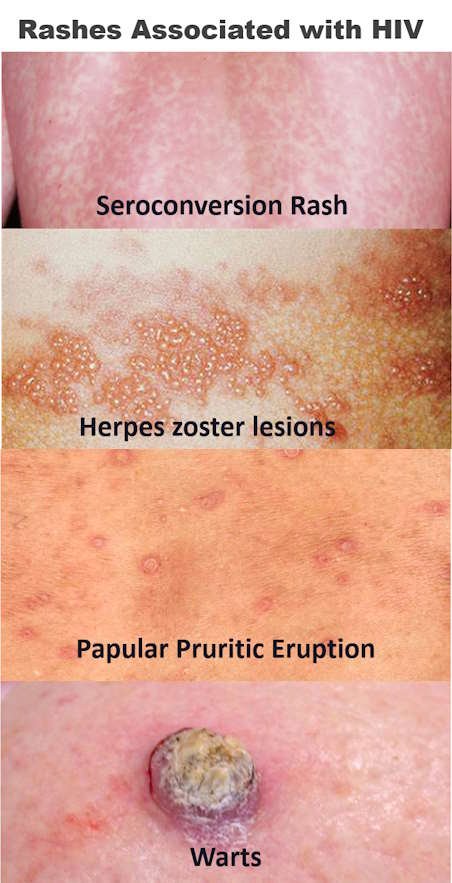
An HIV-specific rash often occurs during the acute phase of HIV infection, also known as seroconversion. This stage typically begins a few days to four weeks after the initial infection. The rash is characterized by widespread, itchy lesions that usually resolve on their own within a few weeks. During this early stage, other symptoms such as fever, fatigue, and swollen lymph nodes may also be present.
What Does an HIV Rash Look Like?
The rash associated with acute HIV infection is typically symmetrical and consists of small, reddish bumps, known as a macular rash. These bumps commonly appear on the trunk, face, limbs, soles of the feet, and palms of the hands. The rash may vary in appearance depending on the individual’s skin tone and the progression of the infection.
Other Symptoms of Early HIV Infection
In addition to the rash, early symptoms of HIV infection, which affect 50-90% of newly infected individuals, may include.
- Fever and Chills. A common sign of many infections, including HIV.
- Sore Throat. Inflammation and pain in the throat, often accompanied by difficulty swallowing.
- Fatigue. Extreme tiredness and lack of energy that is not relieved by rest.
- Lymph Node Enlargement. Swollen lymph nodes, particularly in the neck, armpits, or groin.
- Headache. Persistent pain in the head that may be mild or severe.
- Muscle Pain. Generalized aches and pains in the muscles.
- Mouth Ulcers. Painful sores that can develop on the inside of the mouth or on the gums.
These symptoms typically last for one to three weeks and can be mistaken for the flu or other viral infections. However, if you suspect that you may have been exposed to HIV, it is crucial to seek medical testing and advice.
Common Types of Rashes in HIV Patients
 People living with HIV are prone to various types of rashes, each with different causes and characteristics. These rashes can be a result of antiretroviral therapy (ART), opportunistic infections, or autoimmune responses. Below are some common types of rashes that may affect individuals with HIV.
People living with HIV are prone to various types of rashes, each with different causes and characteristics. These rashes can be a result of antiretroviral therapy (ART), opportunistic infections, or autoimmune responses. Below are some common types of rashes that may affect individuals with HIV.
- Antiretroviral Therapy (ART) Rashes. Some medications used to manage HIV can cause skin reactions. These rashes may present as small, itchy red bumps, hives, or pigmented nail bands, depending on the drug.
- Papular Pruritic Eruption (PPE). This condition is characterized by multiple itchy, firm, and raised bumps on the trunk, limbs, and sometimes the face. The cause of PPE is unknown, but it is commonly seen in HIV patients.
- Herpes Simplex. This rash is caused by the herpes simplex virus (HSV) and appears as grouped, fluid-filled blisters on a red base. It typically affects areas around the mouth, genitals, and anal region. In advanced HIV cases, these blisters can turn into deep sores.
- Herpes Zoster (Shingles). Caused by the varicella-zoster virus, this rash manifests as painful, grouped, fluid-filled blisters on a red base. The rash usually occurs on one side of the body and can merge to form larger blisters.
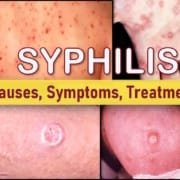
- Syphilis. Primary syphilis presents as a single, painless, firm, round ulcer known as a syphilitic chancre. In HIV patients, syphilis may present atypically, with multiple painful chancres or widespread blistering. Secondary syphilis can cause scaly lesions on the extremities, palms, soles, and mucous membranes.
- Genital and Extra-Genital Warts. Caused by the human papillomavirus (HPV), these warts range from smooth, flattened lesions to cauliflower-like bumps. They can appear on the genital area and other parts of the body, sometimes causing pain, burning, or itching.
- Molluscum Contagiosum. This rash, caused by the molluscum contagiosum virus (MCV), appears as small, flesh-colored bumps with a central dent. In people with advanced HIV, the rash can become widespread and severe.
- Scabies. Scabies is caused by the parasite Sarcoptes scabiei and is characterized by intense itching and small, reddish bumps. A distinctive feature of scabies is the presence of thin, wavy lines on the skin (burrows), which are most commonly found between the fingers, on the wrists, and in other creased areas.
- Thrush. Thrush is a fungal infection caused by Candida albicans, which manifests as non-adherent whitish plaques on the tongue or throat.
- Seborrheic Dermatitis. Caused by the yeast Pityrosporum ovale, this condition results in yellowish, greasy scales on a red or whitish base, commonly appearing on the scalp, face, and upper chest.
- Psoriasis. This autoimmune disease causes thick, white, scaly patches on the skin. In HIV patients, psoriasis may appear as small lesions on the trunk (guttate psoriasis), plaques in skin folds (inverse psoriasis), or widespread redness and scaling (erythrodermic psoriasis).
Severity of HIV Rash
The severity of an HIV-related rash can vary greatly depending on several factors, including the patient’s immune system status, the cause of the rash, and the stage of the disease. In general, patients with advanced HIV infection may experience more severe and widespread rashes. For example.
- Molluscum Contagiosum. This can cause over 100 bumps in advanced HIV patients.
- Scabies. In severe cases, scabies may present as scaling plaques that resemble psoriasis.
- Herpes Zoster and Herpes Simplex. These infections may lead to deep ulcers, scarring, and secondary bacterial infections.
Some rashes associated with HIV can lead to life-threatening complications. One such condition is Stevens-Johnson Syndrome (SJS), which is more common in AIDS patients. SJS is a severe reaction to medications, including some used in ART, and is characterized by red or purple spots that can blister, peel, and resemble severe skin burns. SJS can develop 2-3 weeks after starting treatment and requires immediate medical attention.
Treatment of HIV Rash
An HIV rash can often resolve on its own within a few weeks, but treatment may be necessary if the rash is caused by an infection, medication, or other underlying conditions. Treatment options include.
- Antiretroviral Therapy (ART). ART can significantly improve immune function and reduce the risk of infections that cause rashes. However, if the rash is caused by ART itself, it may be necessary to discuss changing the medication with a healthcare provider.
- Medications. If the rash is related to an STD or another infection, specific treatments such as antibiotics or antiviral drugs may be required. Over-the-counter medications like corticosteroid creams or ointments can help alleviate mild rashes.
- Lifestyle Changes. Avoiding direct sunlight, hot baths, and food allergens can help prevent certain types of rashes. It is also advisable to wear loose-fitting clothing to minimize skin irritation.
Frequently Asked Questions
- How Long Does an HIV Rash Last?
- The rash associated with acute HIV infection typically lasts for about one week, although it may vary depending on individual circumstances.
- How Do I Know if My Rash is Related to HIV?
- The only definitive way to determine if a rash is related to HIV is through medical testing. If you suspect you may have been exposed to HIV, seek testing and medical advice promptly.
- When Should I See a Doctor?
- If you develop a sudden rash and believe you are at risk of HIV infection, it is essential to see a doctor as soon as possible. Early diagnosis and treatment can significantly improve your long-term health outcomes and reduce the risk of transmitting the virus to others.
Conclusion
People living with HIV are susceptible to a variety of skin conditions, some of which can be severe and even life-threatening. While some rashes may resolve on their own or with over-the-counter treatments, it is crucial to seek medical advice for proper diagnosis and management. Early detection and treatment of HIV and related conditions can greatly enhance the quality of life and prevent serious complications.