Gonorrhea: Symptoms, Treatment & Prevention
Gonorrhea, a sexually transmitted infection (STI) caused by the bacterium Neisseria gonorrhoeae, is a significant public health concern worldwide. This infection primarily spreads through vaginal, oral, or anal sex and affects both men and women. Despite its prevalence, many people are unaware of the risks, symptoms, and potential complications associated with gonorrhea. Understanding the key facts about gonorrhea, including how it spreads, its symptoms, diagnosis, treatment and prevention can help you to maintain a healthy life.
What is Gonorrhea?
Gonorrhea is a common sexually transmitted infection caused by the bacterium Neisseria gonorrhoeae. This bacterium thrives in the warm, moist areas of the reproductive tract, including the cervix, uterus, and fallopian tubes in women, and the urethra in both men and women. It can also grow in the mouth, throat, eyes, and anus. The infection is typically spread through sexual contact, including vaginal, oral, and anal sex, with someone who is infected.
How Common is Gonorrhea
Gonorrhea is widespread globally, with the World Health Organization (WHO) estimating that there were approximately 82.4 million new infections among adults aged 15 to 49 years in 2020 alone. The prevalence of gonorrhea is particularly high among vulnerable populations, including men who have sex with men, sex workers, transgender women, and adolescents and young people in high-burden countries. The high rate of infection underscores the importance of awareness, prevention, and timely treatment.
How Does Gonorrhea Spread?
Gonorrhea spreads primarily through sexual contact. You can get gonorrhea by having vaginal, anal, or oral sex without a condom with someone who has the infection. A pregnant person with gonorrhea can also pass the infection to their baby during childbirth. This transmission can lead to serious health complications for the newborn, including eye infections that, if untreated, may lead to blindness.
Symptoms of Gonorrhea
The symptoms of gonorrhea can vary depending on the site of infection genitals, anus, or throat and can differ between men and women. It’s important to note that many people with gonorrhea do not experience any symptoms, which can delay diagnosis and increase the risk of complications. 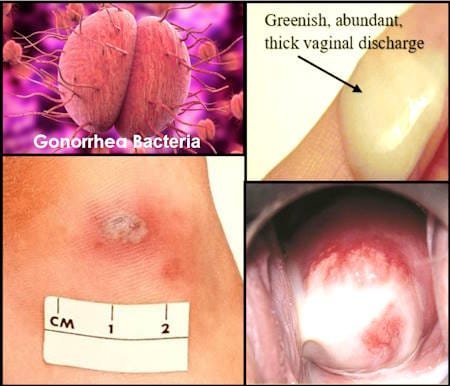
Gonorrhea Symptoms in Men
In men, symptoms usually appear within 1–14 days after exposure. The most common symptoms include:
- Penile Discharge. A white, yellow, or greenish discharge from the penis is a typical sign of gonorrhea.
- Painful Urination. A burning sensation during urination is another common symptom.
- Testicular Pain. Some men may experience pain or swelling in the testicles.
Gonorrhea Symptoms in Women
Most women with gonorrhea do not have symptoms or do not notice them until complications arise. If symptoms do occur, they may include:
- Vaginal Discharge. An unusual discharge from the vagina, which may be white, yellow, or greenish.
- Painful Urination. A burning sensation while urinating.
- Vaginal Bleeding. Bleeding between periods or after sexual intercourse.
Gonorrhea Symptoms in the Anus and Throat
Both men and women can develop gonorrhea in the anus or throat. Symptoms of anal infection may include:
- Discharge from the Anus. A white, yellow, or greenish discharge.
- Itchiness or Soreness. Itching or soreness around the anus.
- Painful Bowel Movements. Discomfort or pain during bowel movements.
Throat infections often have no symptoms, but when they do, they may include:
- Redness and Soreness. A sore throat and redness in the throat.
- Pain. Pain in the throat, especially when swallowing.
Complications of Untreated Gonorrhea
If left untreated, gonorrhea can lead to severe health complications in both men and women. The complications can affect reproductive health, cause systemic infections, and lead to serious conditions.
In Women
Untreated gonorrhea in women can lead to:
- Pelvic Inflammatory Disease (PID). An infection of the female reproductive organs that can cause chronic pelvic pain, ectopic pregnancy, and infertility.
- Ectopic Pregnancy. A potentially life-threatening condition where a fertilized egg implants outside the uterus, often in the fallopian tube.
- Infertility. Permanent damage to the reproductive organs can make it difficult or impossible for a woman to become pregnant.
In Men
Men with untreated gonorrhea may experience:
- Scrotal Swelling. Inflammation of the epididymis (a tube at the back of the testicles), which can cause pain and swelling.
- Urethral Stricture. A narrowing of the urethra, which can cause difficulty urinating.
- Infertility. In severe cases, gonorrhea can lead to infertility in men.
In Newborns
Infants born to mothers with gonorrhea are at risk of developing:
- Neonatal Conjunctivitis: An eye infection that can cause redness, pain, soreness, ulcers, and tearing. If untreated, it can lead to blindness.
Systemic Complications
In rare cases, gonorrhea can spread to other parts of the body, leading to disseminated gonococcal infection (DGI). DGI can cause:
- Fever: A high temperature indicating an infection in the body.
- Joint Pain and Swelling: Inflammation of the joints, leading to pain and swelling.
- Skin Sores: Ulcers or sores on the skin.
- Heart and Meninges Infection: Infection of the heart (endocarditis) or the membranes covering the brain and spinal cord (meningitis).
The Impact of Gonorrhea on Mental Health
In addition to physical complications, gonorrhea can also have significant emotional and psychological effects. The stigma associated with sexually transmitted infections can lead to feelings of shame, embarrassment, and isolation. These feelings can strain personal relationships and contribute to mental health issues such as anxiety and depression. It’s important for individuals diagnosed with gonorrhea to seek support from healthcare providers, counselors, or support groups to address these emotional challenges.
Diagnosis of Gonorrhea
Early diagnosis of gonorrhea is crucial for preventing complications and stopping the spread of the infection. There are several methods used to diagnose gonorrhea:
- Gonorrhea Molecular Tests. Molecular tests, also known as nucleic acid amplification tests (NAATs), are the gold standard for diagnosing gonorrhea. These tests detect the genetic material of Neisseria gonorrhoeae and can be performed on urine samples, swabs from the genital area, anus, throat, or eyes. Molecular tests are highly accurate and can be done in a laboratory or at the point of care.
- Gram Stain Microscopy. Gram stain microscopy is another diagnostic method used in some laboratories. This method involves staining a sample of discharge or tissue and examining it under a microscope. While this method can be useful, it is less sensitive in women and for detecting throat and anal infections.
- Syndromic Approach. In settings where diagnostic testing is not available, healthcare providers may use a syndromic approach to manage gonorrhea cases. This approach involves evaluating symptoms and risk factors to make a presumptive diagnosis and begin treatment.
- Screening and Risk Assessment. Because many people with gonorrhea do not have symptoms, routine screening is recommended for individuals at higher risk, such as sexually active adolescents, men who have sex with men, and sex workers. Screening is often done in conjunction with tests for other sexually transmitted infections, such as HIV, syphilis, and chlamydia.
- Antimicrobial Sensitivity Testing. In cases where treatment fails, antimicrobial sensitivity testing may be performed to determine if the Neisseria gonorrhoeae strain is resistant to the prescribed antibiotics. Monitoring antibiotic resistance patterns is essential for guiding treatment recommendations and managing the spread of resistant strains.
Treatment of Gonorrhea
Gonorrhea is treatable and can be cured with antibiotics. However, the emergence of antibiotic-resistant strains of Neisseria gonorrhoeae has made treatment more challenging. For treating uncomplicated gonorrhea in adults and adolescents, the recommended approach varies depending on the site of infection, and whether there is a co-existing chlamydial infection.
Infection of the Cervix, Urethra, or Rectum
The preferred treatment for an uncomplicated gonorrhea infection in the cervix, urethra, or rectum is a single injection of ceftriaxone, with the dosage based on body weight:
- For individuals weighing less than 150 kg (330 lbs): Ceftriaxone 500 mg is given as an intramuscular (IM) injection in a single dose.
- For individuals weighing 150 kg (330 lbs) or more: Ceftriaxone 1 g should be administered as a single IM injection.
If there’s a possibility of a co-existing chlamydia infection, but it hasn’t been ruled out, it’s important to treat for chlamydia as well. In this case, patients should take:
- Doxycycline 100 mg, taken orally twice a day for 7 days.
Ceftriaxone is highly effective for treating gonorrhea, including at urogenital sites like the cervix, urethra, and rectum. A single dose of 500 mg typically maintains a sufficient drug concentration to clear the infection for around 50 hours, which is adequate for most cases.
Alternative Treatments
If a patient has an allergy to cephalosporins (the class of antibiotics that includes ceftriaxone), or if ceftriaxone is not available, alternative regimens can be considered:
- Gentamicin 240 mg as a single IM injection, plus Azithromycin 2 g taken orally in a single dose.
Another option, if ceftriaxone cannot be administered for other reasons, is:
- Cefixime 800 mg taken orally in a single dose.
As with the standard treatment, if chlamydia hasn’t been excluded, add doxycycline for 7 days.
Infection of the Throat (Pharyngeal Gonorrhea)
Gonorrhea in the throat (pharyngeal gonorrhea) is more challenging to treat than infections in other areas like the genital or rectal regions. Although pharyngeal gonorrhea is often asymptomatic, it can be a significant source of transmission and may contribute to antibiotic resistance. It’s important for healthcare providers to ask patients with genital or rectal gonorrhea if they’ve had oral sex, and to test the throat if necessary.
For treating uncomplicated pharyngeal gonorrhea, the recommended treatment is:
- Ceftriaxone 500 mg as a single IM injection for individuals weighing less than 150 kg (330 lbs).
- Ceftriaxone 1 g for those weighing 150 kg or more.
If a chlamydial infection is also present, add doxycycline 100 mg, taken orally twice a day for 7 days.
Currently, there are no reliable alternative treatments for pharyngeal gonorrhea. If a patient has a severe allergy (such as anaphylaxis or Stevens-Johnson syndrome) to ceftriaxone, an infectious disease specialist should be consulted to determine an alternative treatment.
Gonorrhea Antibiotic Resistance
One of the most concerning developments in the treatment of gonorrhea is the rise of antibiotic-resistant strains of Neisseria gonorrhoeae. Over the years, the bacterium has developed resistance to many antibiotics, making treatment increasingly difficult. The World Health Organization has identified antibiotic resistance in gonorrhea as a serious global health threat.
Treatment Failure
Treatment for gonorrhea may fail for several reasons:
- Incorrect Use of Medications: Not taking the antibiotics as directed can lead to treatment failure.
- Reinfection: A person can be reinfected with gonorrhea if they are exposed to the bacteria again.
- Antibiotic Resistance: The bacterium may be resistant to the prescribed antibiotic, rendering the treatment ineffective.
- Coinfection with Another STI: Having another untreated STI with similar symptoms can complicate treatment.
After treatment, it is recommended to wait seven days before having sex and to notify sexual partners so they can be tested and treated if necessary. It is also important to complete the full course of antibiotics, even if symptoms disappear before finishing the medication.
Gonorrhea Prevention
Prevention is the best approach to managing gonorrhea. Here are some strategies to reduce the risk of infection:
- Condom Use. Consistent and correct use of condoms during every sexual encounter is highly effective in preventing gonorrhea and other sexually transmitted infections.
- Monogamous Relationships. Being in a long-term mutually monogamous relationship with a partner who has been tested and is free of gonorrhea can reduce the risk of infection.
- Routine Screening. Sexually active individuals, especially those with multiple partners, should undergo regular screenings for gonorrhea and other STIs. Early detection and treatment can prevent complications and the spread of infection.
- Partner Notification. Individuals diagnosed with gonorrhea should inform their current and recent sexual partners so they can be tested and treated if necessary. This helps to prevent the spread of the infection and reduce the risk of reinfection.
- Protecting Newborns. Pregnant women should be screened and treated for gonorrhea to protect their babies from infection during childbirth. Newborns at risk of exposure to gonorrhea should receive antibiotic eye ointment to prevent eye infections.
FAQs: Gonorrhea – Transmission, Symptoms, and Treatment
Can gonorrhea be spread through kissing?
While gonorrhea is primarily transmitted through sexual contact, it can potentially be spread through kissing in rare cases. The bacteria can infect the throat, and deep kissing with an infected person might lead to transmission. However, this is much less common than transmission through genital, anal, or oral sexual contact.
How can I differentiate between oral gonorrhea and strep throat?
Oral gonorrhea and strep throat can have similar symptoms, making them difficult to distinguish without proper testing. Both can cause a sore throat, swollen lymph nodes, and fever. However, oral gonorrhea is typically associated with sexual activity, while strep throat is usually spread through respiratory droplets. Always consult a healthcare provider for an accurate diagnosis.
Is amoxicillin effective for treating gonorrhea?
Amoxicillin is no longer recommended as a first-line treatment for gonorrhea due to widespread antibiotic resistance. Current guidelines suggest using other antibiotics, such as ceftriaxone, often in combination with azithromycin. Always follow your healthcare provider’s prescription, as treatment recommendations may change based on local resistance patterns.
How is doxycycline used in gonorrhea treatment?
Doxycycline is sometimes used as part of a dual therapy approach for treating gonorrhea, often in combination with other antibiotics like ceftriaxone. It’s particularly useful in treating potential co-infections with chlamydia. However, the specific treatment plan should always be determined by a healthcare provider based on current guidelines and individual patient factors.
Can metronidazole treat both gonorrhea and chlamydia?
Metronidazole is not typically used to treat gonorrhea or chlamydia. It’s primarily effective against certain anaerobic bacteria and parasites. For gonorrhea and chlamydia, other antibiotics such as ceftriaxone, azithromycin, or doxycycline are usually prescribed. Always consult with a healthcare provider for appropriate treatment.
What are the symptoms of gonorrhea in the mouth or tongue (oral gonorrhea) ?
Gonorrhea in the tongue or mouth (oral gonorrhea) may cause symptoms such as a sore throat, redness or swelling in the mouth, and occasionally, white spots on the tonsils. However, many people with oral gonorrhea don’t experience any symptoms. Regular testing is important if you’re at risk, even if you don’t have symptoms.
Can gonorrhea remain dormant in the body?
Gonorrhea can be asymptomatic, meaning a person can have the infection without showing any signs. This is often referred to as “dormant” gonorrhea. However, even without symptoms, the bacteria are active and can cause complications if left untreated. Regular testing is crucial, especially for those at higher risk.
Are home testing kits available for gonorrhea?
Yes, home testing kits for gonorrhea are available. These typically involve collecting a urine sample or a swab, which you then send to a lab for analysis. While convenient, it’s important to follow up with a healthcare provider for any positive results, as proper treatment and partner notification are crucial.
Does gonorrhea cause a noticeable odor?
Gonorrhea itself doesn’t typically cause a strong odor. However, it can lead to changes in vaginal or penile discharge, which might have a slight odor. A strong, fishy odor is more commonly associated with bacterial vaginosis. If you notice any unusual odors or discharge, it’s best to consult a healthcare provider.
Can gonorrhea affect the eyes?
Yes, gonorrhea can affect the eyes, causing a condition called gonococcal conjunctivitis. This can occur when infected fluids come into contact with the eyes. Symptoms may include redness, pain, swelling, and discharge. This condition requires immediate medical attention to prevent serious complications.
How common is it to have both gonorrhea and chlamydia at the same time?
Co-infection with gonorrhea and chlamydia is relatively common. Both are sexually transmitted infections that can be acquired simultaneously. Due to this frequent co-occurrence, many healthcare providers treat for both infections when either is diagnosed. Regular testing for both infections is recommended for sexually active individuals.
Conclusion
Gonorrhea is a common but serious sexually transmitted infection that can have significant health consequences if left untreated. While it is curable with antibiotics, the rise of antibiotic-resistant strains poses a growing challenge. Awareness, prevention, early diagnosis, and responsible treatment are crucial in managing this infection. By practicing safe sex, getting regular screenings, and following prescribed treatments, individuals can protect themselves and others from the harmful effects of gonorrhea. If you suspect you may have gonorrhea or have been exposed to it, seek medical advice promptly to receive the appropriate care.










