Fungal Infection: Types, Causes & Treatments
Fungal infections are more common than you might think, affecting millions of people worldwide. While fungi are essential components of our environment and play many beneficial roles, they can also lead to a range of infections when they overgrow or invade our bodies. Despite being less discussed compared to bacterial or viral infections, fungi can cause a variety of health issues, ranging from mild irritations to severe systemic infections. Understanding how these infections occur, their symptoms, and effective treatment options is crucial for maintaining good health.
What Are Fungal Infections?
Fungal infections, or mycosis, are diseases caused by fungi, which are microorganisms distinct from plants and animals. These infections can affect the skin, hair, nails, and mucous membranes, but they can also invade deeper tissues such as the lungs, blood, and organs. While many fungi are harmless and live naturally on or inside the body, certain types can cause infections when they overgrow or enter the body through breaks in the skin.
Understanding Fungi
Fungi are a diverse group of organisms that can be found in various environments, including soil, water, and on the surface of living organisms. They reproduce by releasing spores, which can be spread through the air or come into contact with surfaces. While millions of fungal species exist, only a few are pathogenic (disease-causing) to humans.
Fungi can be categorized into several types:
- Yeasts: Single-celled fungi that can cause infections like candidiasis.
- Molds: Multicellular fungi that often grow in filaments and can lead to conditions like aspergillosis.
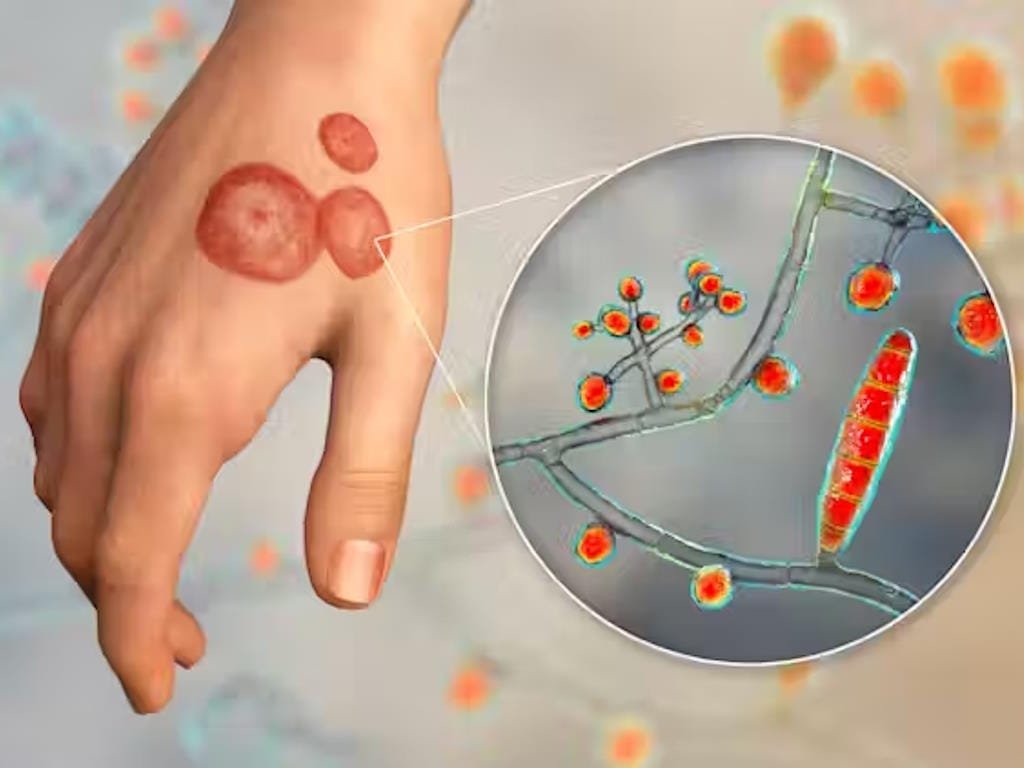
- Dermatophytes: Fungi that infect skin, hair, and nails, causing conditions such as ringworm.
Identifying Fungal Infections
Fungal infections can present in various ways, depending on their location and the type of fungus involved. Common signs include:
- Skin: Redness, swelling, rash, or lumps. Fungal infections might cause peeling or cracking of the skin.
- Nails: Discoloration (yellow, brown, or white), thickening, or brittleness.
- Mouth/Throat: White patches or coating, pain, and difficulty swallowing.
- Lungs: Cough, shortness of breath, fever, and chest pain.
- Vagina: Discomforting symptoms such as itching, burning sensations, and abnormal vaginal discharge. For more information see “Vaginal Yeast Infections: Symptoms, Causes and Treatmentn“.
Risk Factors for Fungal Infections
While anyone can develop a fungal infection, certain risk factors for fungal infections can increase your likelihood of developing these conditions by creating an environment in which fungi can thrive or by compromising your body’s ability to fight infections. Here are key risk factors to be aware of:
- Weakened Immune System. A weakened immune system significantly increases the risk of fungal infections. Individuals with conditions such as HIV/AIDS, cancer, or those undergoing chemotherapy or taking immunosuppressive medications have compromised immune responses. This diminished ability to fend off infections allows fungi to proliferate more easily and cause illness.
- Diabetes. Diabetes creates an environment that can promote fungal growth due to high blood sugar levels. Elevated glucose can foster fungal overgrowth, particularly in areas like the skin and mucous membranes. Additionally, diabetes can impair the body’s immune response, making it harder to combat infections.
- Use of Antibiotics and Corticosteroids. Long-term use of certain medications, such as antibiotics and corticosteroids, can disrupt the body’s natural balance of microorganisms. This disruption often leads to fungal overgrowth as the balance between different types of microorganisms is altered, allowing fungi to thrive
- Damp and Humid Conditions. Fungi thrive in warm, moist environments, making individuals exposed to such conditions more susceptible to fungal infections. Excessive sweating, living in humid climates, or prolonged exposure to damp conditions can create ideal environments for fungal growth and infection.
- Poor Blood Circulation. Poor blood circulation, often seen in conditions like diabetes or peripheral artery disease, reduces the body’s ability to deliver immune cells to areas where infections may occur. This compromised blood flow can make it more difficult for the body to fight off fungal infections and heal affected areas.
- Menopausal Status. During menopause, hormonal changes can lead to a decrease in vaginal acidity, which normally helps to inhibit fungal growth. This reduction in acidity can increase the risk of developing vaginal yeast infections, as fungi like Candida can flourish in a less acidic environment.
- Skin and Nail Injuries. Injuries to the skin or nails can provide an entry point for fungi to invade and cause infections. Cuts, abrasions, or trauma to these areas compromise the natural barrier that protects against fungal invasion, making it easier for fungi to penetrate and infect.
- Age. Both very young children and older adults are at higher risk for fungal infections due to differences in immune system efficacy. Young children have developing immune systems, while older adults may have weakened immune responses, both making them more vulnerable to fungal infections.
- Lifestyle Factors. Lifestyle factors such as wearing tight or non-breathable clothing, especially in warm and humid conditions, can increase the risk of fungal infections. Activities that involve shared environments like public showers, swimming pools, or gyms can also expose individuals to fungal spores and increase the risk of infection.
- Underlying Health Conditions . Chronic health conditions like asthma, chronic obstructive pulmonary disease (COPD), or kidney disease can increase susceptibility to fungal infections. These conditions can impair the body’s overall ability to handle infections, making individuals more prone to fungal invasions.
Types of Fungal Infections
Fungal infections are generally classified based on their location in the body:
1. Superficial Fungal Infections
These affect the outer layers of the skin, nails, and mucous membranes:
- Ringworm: Caused by dermatophytes, leading to circular, itchy rashes on the skin or scalp.
- Onychomycosis: Fungal infection of the nails, causing discoloration and thickening.
- Candidiasis: Infections caused by Candida species, affecting the mouth (oral thrush), genitals (vaginal yeast infections), and skin.
- Tinea Versicolor: Caused by the Malassezia fungus, resulting in discolored patches on the skin.
2. Subcutaneous Fungal Infections
These occur beneath the skin, often through injuries:
- Sporotrichosis: Known as rose gardener’s disease, typically contracted from thorns or soil.
- Chromoblastomycosis: Chronic skin infection that can spread from the initial site.
- Eumycetoma: Often affects the feet, causing swelling and abscesses.
3. Deep Fungal Infections
These infections affect internal organs and are more serious:
- Histoplasmosis: Affects the lungs and sometimes other organs, commonly found in the Ohio and Mississippi River valleys.
- Coccidioidomycosis: Also known as Valley fever, prevalent in California and Arizona.
- Blastomycosis: Affects the lungs, skin, and bones, with rare cases involving the brain.
- Aspergillosis: Caused by Aspergillus molds, leading to lung infections and sometimes affecting other parts of the body.
- Cryptococcosis: Caused by Cryptococcus fungi, which can infect the lungs and brain.
- Mucormycosis: Affects various body parts including the sinuses and brain, particularly in those with weakened immune systems.
- Pneumocystis Pneumonia (PJP): A lung infection commonly seen in immunocompromised individuals.
Symptoms and Causes of Fungal Infections
Symptoms vary based on the type of infection and its location. Common symptoms include:
- Skin and Nails: Itching, redness, scaling, and changes in nail texture.
- Lungs: Persistent cough, shortness of breath, fever, and fatigue.
- Mouth and Throat: White patches, sore throat, and difficulty swallowing.
- Other Organs: Headaches, abdominal pain, or visual disturbances depending on the affected organ.
Fungal infections are generally caused by exposure to fungi from the environment or a disruption in the natural balance of microorganisms on the body. Transmission can occur through:
- Direct Contact: From an infected person or animal.
- Environmental Exposure: From soil, dust, or contaminated surfaces.
- Injuries: Through cuts or wounds, particularly when working with soil or plants.
Diagnosis and Tests
Diagnosing a fungal infection involves:
- Physical Examination: Assessing visible symptoms on the skin or nails.
- Lab Tests: Analyzing samples from affected areas (skin, nails, blood, etc.) to identify the fungus.
- Imaging: X-rays, CT scans, or MRIs may be used for internal infections.
Fungal Infections Treatment Options
Treatment depends on the type and severity of the infection:
- Topical Antifungals: Creams, ointments, powders and sprays for skin and nail infections.
- Oral Antifungals: Pills or liquid medications for more severe or widespread infections.
- Intravenous Antifungals: Administered in a hospital for severe systemic infections.
- Specialized Treatments: Such as antifungal mouthwash for oral thrush or shampoos for scalp infections.
Fungal Infections Prevention
Preventing fungal infections involves good hygiene and avoiding environments where fungi thrive. Key strategies include:
- Keep Skin Dry: Fungi thrive in moist environments, so ensure skin is thoroughly dried, especially in prone areas.
- Practice Good Hygiene: Wash hands frequently, especially after touching animals or other people.
- Avoid Sharing Personal Items: Don’t share towels, razors, or other personal care items.
- Disinfect Common Areas: Clean and disinfect gym equipment and other shared surfaces.
- Avoiding Contaminated Areas: Such as public showers and swimming pools.
- Proper Wound Care: Treating cuts and injuries promptly.
- Safe Use of Medications: Using antibiotics only as prescribed.
- Protective Clothing: Wearing appropriate gear when handling soil or working in dusty environments.
Prognosis and Living with Fungal Infections
Most superficial fungal infections can be managed effectively with treatment, although they may take time to fully resolve. Deep fungal infections can be more serious and require prompt medical attention, particularly in individuals with weakened immune systems. Regular follow-ups with healthcare providers are essential to ensure successful treatment and prevent complications.
When to See a Healthcare Provider
Seek medical attention if you experience symptoms of a fungal infection that do not improve with over-the-counter treatments or if you have a weakened immune system and develop signs of a serious infection. Your healthcare provider can offer personalized advice and treatment options based on your condition.
Conclusion
Fungal infections are a widespread health issue that can range from minor inconveniences to serious health concerns. Understanding the types, symptoms, and treatment options for fungal infections can help you manage and prevent these conditions effectively. If you suspect you have a fungal infection, consult your healthcare provider for a proper diagnosis and treatment plan.