Breast Cancer: Types, Symptoms & Treatment
Breast cancer is a condition where cells in the breast grow uncontrollably, usually starting in milk-producing glands (lobules) or milk-carrying ducts. Among women, breast cancer is one of the most commonly diagnosed cancers. Early detection and treatment significantly improve outcomes, making awareness of symptoms, risk factors, and treatment options essential for patients and families alike.
What is Breast Cancer?
Breast cancer begins when cells in the breast become abnormal, growing and dividing uncontrollably. It commonly starts in the milk-producing glands (lobules) or the ducts that carry milk to the nipple. Among women, it’s one of the most frequent cancer types, with the first symptom often being a painless lump that’s usually self-detected. If a lump is found, a biopsy is performed—where tissue is taken, often via a needle or small incision, and examined under a microscope.
Most breast disorders are benign and don’t need treatment, while breast cancer can be life-threatening or result in breast removal. To catch potential issues early, women should have regular physical exams, follow mammogram recommendations, and stay familiar with the normal look and feel of their breasts. Men can also develop breast cancer, so they too should monitor for any changes around the nipple area.
How Common is Breast Cancer
Global Statistics: In 2022, breast cancer affected 2.3 million women globally, resulting in approximately 670,000 deaths. This cancer occurs in all countries and can affect women at any age after puberty, with incidence rates rising as women age. Breast cancer is one of the most prevalent cancers worldwide, impacting women of all backgrounds.
United States Statistics: In 2023, it is projected that 297,790 new cases of invasive breast cancer and 55,720 cases of noninvasive (in situ) breast cancer will be diagnosed in women in the United States. Additionally, breast cancer is expected to cause 43,700 deaths among women. Among men, there are an estimated 2,800 new cases of invasive breast cancer and 530 deaths attributed to the disease.
Breast Cancer Risk Factors
Breast cancer risk is influenced by genetics, lifestyle, and age. While age and certain genetic factors, such as BRCA mutations, can’t be changed, factors like regular exercise and limited alcohol intake can reduce risk. Major risk factors include:
- Age: Highest rates are in women aged 65-74.
- Family History: Risk doubles with a first-degree relative with breast cancer.
- BRCA Gene Mutations: BRCA1 and BRCA2 mutations, more common among Ashkenazi Jewish people, significantly increase lifetime risk. Men with BRCA mutations also have a slightly elevated risk.
- Breast Density: Dense tissue can increase risk and complicate detection.
- Hormone Therapy: Post-menopause hormone therapy with estrogen and progestin can increase risk.
- Previous Breast Cancer History: Having had breast cancer previously raises recurrence risk.
Types of Breast Cancer
Breast cancer is classified by the tissue where it starts and its spread level. Common types include:
- Ductal Carcinoma: Starts in milk ducts and accounts for about 90% of cases.
- Lobular Carcinoma: Begins in milk-producing glands.
- Paget Disease of the Breast: Affects the nipple area, presenting as crusty or scaly sores with potential discharge.
- Phyllodes Tumors: Rare, originating in breast tissue around milk ducts, and can metastasize.
- Inflammatory Breast Cancer: A particularly aggressive form, inflammatory breast cancer causes swelling, redness, and warmth in the breast due to cancer cells blocking lymphatic vessels. It often spreads to lymph nodes and appears without a distinct lump.
Metastasis and Spread
Breast cancer can spread through lymphatic vessels, commonly affecting bones, liver, brain, and lungs. If it’s found in one area, it often indicates spread to others, which might go undetected for years. Breast cancer is commonly classified into two main types:
Carcinoma in situ
This refers to early-stage breast cancer, where the cancer remains “in place” without invading nearby tissues or spreading to other areas of the body. Carcinoma in situ can grow significantly within the breast but is non-invasive at this stage.
- Ductal Carcinoma in Situ (DCIS): The most common form of carcinoma in situ, DCIS is restricted to the milk ducts. While it may spread within the ducts, it doesn’t invade surrounding tissues, though it can eventually become invasive. It comprises around 85% of carcinoma in situ cases and is often detected through mammography.
- Lobular Carcinoma in Situ (LCIS): LCIS forms within the milk-producing glands (lobules) and may develop in multiple areas of both breasts. Women with LCIS have a 1-2% annual risk of developing invasive breast cancer in either breast. Unlike DCIS, LCIS is typically undetectable on mammograms and is usually identified through biopsy. LCIS has two forms: the classic type, which is non-invasive but increases cancer risk, and the pleomorphic type, which is invasive and often surgically removed upon detection.
Invasive Cancer
This type of breast cancer has spread beyond the breast tissue. It can be further categorized by the extent of its spread:
- Localized: Confined to the breast only.
- Regional: Spread to nearby areas, like the chest wall or lymph nodes.
- Distant (Metastatic): Cancer has spread to other parts of the body.
Common invasive types include:
- Invasive Ductal Carcinoma (IDC): Originates in the milk ducts and breaks through to surrounding tissue, often spreading to other areas. IDC accounts for about 75% of invasive breast cancers.
- Invasive Lobular Carcinoma (ILC): Begins in milk-producing glands, invades surrounding breast tissue, and often appears in both breasts. It makes up most of the remaining cases of invasive breast cancer.
Rare types of invasive breast cancers, such as medullary, tubular, metaplastic, and mucinous carcinoma, present varying prognoses. Metaplastic and inflammatory breast cancers are usually aggressive, while medullary, mucinous, cribriform, and tubular carcinomas often have better outcomes. Mucinous carcinoma generally develops in older women and grows slowly.
Tumor Receptors
Breast cancer cells, like all cells, have surface molecules called receptors. These receptors influence cell behavior, including cancer growth and spread, and can guide treatment approaches. Key receptors include:
- Estrogen and Progesterone Receptors: Estrogen receptor-positive breast cancers are stimulated by estrogen and grow more slowly, often with a better prognosis. About 80% of postmenopausal and 20% of premenopausal women with breast cancer have estrogen receptor-positive cancer. Progesterone receptor-positive cancers, similarly, are influenced by progesterone and comprise about 70% of breast cancers.
- HER2 Receptors: HER2-positive breast cancers involve overexpression of HER2 receptors, making them more aggressive and fast-growing. About 15% of breast cancers are HER2-positive.
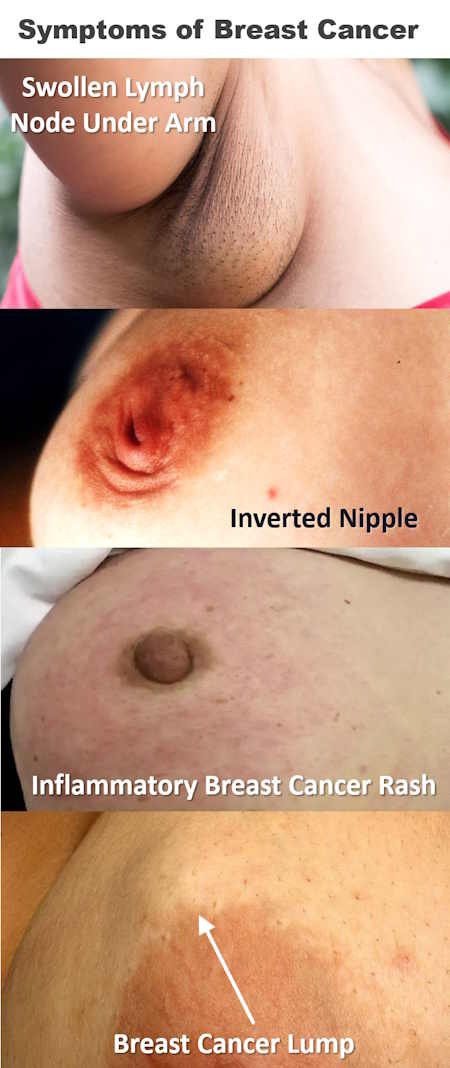
Breast Cancer Symptoms
Early breast cancer often shows no symptoms. A common initial sign is a painless lump. Other symptoms include:
- Breast pain (though not common) can occasionally accompany breast cancer.
- Bloody nipple discharge, especially from a single breast, can be concerning.
- Lumps or thickened areas that differ from surrounding tissue may appear as firm masses.
- Attachment of the lump to skin or chest wall can indicate advanced stages.
- Swelling or skin changes, such as dimpling or a leathery texture, may appear as the cancer progresses.
Advanced cancer may also result in swollen lymph nodes in the armpit or distant symptoms if it spreads to bones (causing ache or weakness) or lungs (causing cough or breathing difficulty).
Diagnosis of Breast Cancer
Breast cancer is commonly diagnosed through:
- Imaging Tests: Initial screening through mammography or breast MRI helps identify abnormalities. If a mass is suspected, ultrasonography distinguishes cysts from solid lumps. MRI may guide biopsies if abnormalities are present only on MRI.
- Biopsy Types:
- Core Needle Biopsy: Removes tissue samples using a hollow needle.
- Open Biopsy: Used when needle biopsy is impractical, involves a small incision to remove part or all of a lump.
- Stereotactic Biopsy: Especially helpful for targeting micro calcifications, stereotactic biopsy uses mammograms to guide biopsy location in three dimensions.
A pathologist examines biopsy samples under a microscope to confirm the presence of cancer cells.
- Evaluation Post-Diagnosis: Following diagnosis, specialists such as surgeons, medical oncologists, and radiation oncologists conduct further evaluations to determine cancer characteristics, including hormone receptor presence, HER2 receptor levels, and cell division rates. Genetic testing may also be conducted for certain breast cancers.
After a breast cancer diagnosis, doctors may order several tests, including:
- A chest x-ray to assess whether the cancer has spread.
- Blood tests like a complete blood count (CBC), liver function tests, and calcium levels to detect metastasis.
- Genetic testing (through blood or saliva) in women with a family history of breast cancer or inherited gene mutations, such as BRCA mutations.
- Bone scans, CT scans of the abdomen and chest, or MRI imaging as needed.
- Blood tests for cancer markers, substances produced by cancer cells, are sometimes ordered.
The National Comprehensive Cancer Network (NCCN) recommends genetic testing for certain women with a current or past breast cancer diagnosis to detect gene mutations linked to increased risk. Some experts suggest that all breast cancer patients undergo genetic testing. Genetic counselors are often involved, documenting family cancer history, selecting tests, and interpreting results.
Staging of Breast Cancer
Upon diagnosis, breast cancer is assigned a stage from 0 to IV (with some substages indicated by letters) based on how widespread and aggressive the cancer is:
- Stage 0: In situ breast cancer, such as ductal carcinoma in situ, indicates cancer confined to its origin without spreading to surrounding tissues.
- Stages I-III: Cancer has spread within or near the breast (localized or regional).
- Stage IV: Metastatic breast cancer, meaning it has spread to other body parts.
Cancer staging assists doctors in determining treatment and prognosis. Factors influencing stage assignment include:
- Cancer size.
- Spread to lymph nodes.
- Metastasis to organs like the lungs or brain.
Other staging factors include:
- Grade: The level of abnormality in cancer cells, from 1 to 3.
- Hormone receptor status: Presence of estrogen, progesterone, and/or HER2 receptors in cancer cells.
- Genetic profile: Tests like Oncotype DX identify gene mutations affecting cancer behavior.
Cancers with cells resembling normal cells are well-differentiated and generally grow slowly, while poorly differentiated cancers grow and spread more aggressively. Receptor status and gene mutations impact treatment response and prognosis.
Treatment of Breast Cancer
Breast cancer treatment options include:
- Surgery
- Radiation therapy
- Systemic chemotherapy
- Hormone blockers
Treatment planning follows a detailed assessment of the cancer’s type, stage, and receptor status. Since breast cancer varies in growth rates, metastasis risk, and treatment responses, doctors may have differing recommendations. Decision-making involves a shared process, where patients receive clear explanations of what is known about their cancer and available treatments. This allows them to weigh options and make informed choices.
Women may be invited to participate in clinical trials for new treatments aimed at improving survival or quality of life. It is crucial to understand the risks and benefits before participating.
Most breast cancer treatments involve surgery, often combined with radiation, chemotherapy, or hormone blockers. Surgery options may include partial or full breast removal (mastectomy), depending on tumor size and location. Some women may opt for breast-conserving surgery, which allows for tumor removal while retaining breast tissue. Plastic or reconstructive surgeons are often involved, particularly for reconstruction in the same operation.
Surgery Options
Two main surgery types are:
- Breast-conserving surgery (plus radiation therapy): Tumor removal with surrounding tissue to reduce recurrence.
- Mastectomy (breast removal): Options vary in the extent of tissue removed.
Invasive cancers (Stage I or higher) may be treated as effectively with breast-conserving surgery plus radiation as with mastectomy if the tumor can be fully removed. Breast-conserving surgery aims to retain as much of the breast as possible. Radiation therapy often follows surgery, reducing the risk of cancer returning.
Types of Mastectomy
- Skin-sparing mastectomy: Preserves muscle under the breast and some skin for easier reconstruction.
- Nipple-sparing mastectomy: Keeps the nipple and surrounding areola.
- Simple mastectomy: Leaves the underlying muscle and armpit lymph nodes.
- Modified radical mastectomy: Removes some armpit lymph nodes, sparing the breast’s underlying muscle.
- Radical mastectomy: Removes both armpit lymph nodes and the muscle under the breast, used only if cancer invades muscle tissue.
Lymph Node Assessment
Lymph node evaluation is essential to determine whether cancer has spread beyond the breast. The lymphatic system drains fluid from breast tissue and traps foreign or abnormal cells, including cancer cells. Cancerous lymph nodes may indicate cancer spread, influencing treatment planning.
Methods of lymph node assessment include:
- Ultrasonography: Checks for enlarged lymph nodes in the armpit.
- Biopsy: Fine-needle or core needle biopsy collects tissue for analysis.
- Axillary lymph node dissection: Removes multiple lymph nodes for examination.
- Sentinel lymph node dissection: Identifies and removes the first lymph node(s) likely to contain cancer cells.
If doctors detect enlarged lymph nodes in the armpit, they may use ultrasonography to guide a needle biopsy. Cancer detected in these nodes may warrant axillary lymph node dissection, although removing many lymph nodes does not necessarily improve the cure rate. This step is primarily diagnostic, helping to guide treatment options.
In cases where cancer is not found in biopsy samples, a sentinel lymph node biopsy may be done. This technique allows doctors to assess the first lymph node affected by cancer. Using a blue dye and/or radioactive substance, they trace the pathway to the sentinel lymph node, removing it to check for cancer. If cancer is absent, additional lymph nodes are not removed.
Surgical removal of lymph nodes can lead to complications, such as fluid buildup and persistent swelling (lymphedema) in the arm or hand. Lymphedema risk persists throughout life, potentially affecting arm and shoulder mobility. Physical therapy may be necessary, and specialized massage techniques can assist in managing fluid buildup. The arm should remain active to avoid exacerbating symptoms.
Patients may be advised to avoid catheter or needle insertions and blood pressure measurements in the affected arm. Preventive measures like wearing gloves when handling items that could cause injury can help manage lymphedema risk. Other potential complications of lymph node removal include numbness, persistent burning sensations, and infection.
Breast Reconstruction Surgery: Options and Timing
Breast reconstruction can take place during a mastectomy or be delayed. Consulting with a plastic surgeon early in treatment planning is essential, as the timing of reconstruction often depends on other necessary treatments. For example, radiation therapy before reconstruction may limit surgical options. Oncoplastic breast surgery, which combines cancer removal with aesthetic techniques, is one option to preserve or restore breast appearance.
Common breast reconstruction techniques include:
- Implants – typically silicone or saline.
- Tissue Flap Surgery – using tissue from other parts of the body (often the abdomen) to reconstruct the breast.
A tissue expander may be placed under the chest muscle during mastectomy to gradually stretch the skin and muscle for an implant. This expander is later removed, and an implant is inserted.
For a more natural reconstruction, tissue from areas like the abdomen, back, or buttock can be used to create a breast shape. Nipple and areola reconstruction typically occurs in a later procedure, sometimes using tattooing or tissue from other body areas.
Contralateral Prophylactic Mastectomy (Preventive Breast Removal)
In some cases, women with a high risk of developing cancer in the opposite breast may opt for a preventive mastectomy (contralateral prophylactic mastectomy). This option may be suggested for those with:
- A genetic mutation (e.g., BRCA1 or BRCA2) that increases cancer risk
- Multiple family members with breast or ovarian cancer
- Prior radiation therapy to the chest before age 30
- Noninvasive breast conditions like lobular carcinoma in situ (LCIS)
Benefits include a lower need for regular imaging tests and potentially extended survival for high-risk women. However, the procedure carries a higher risk of complications.
Radiation Therapy in Breast Cancer Treatment
Radiation therapy is commonly used to kill cancer cells remaining after tumor removal. Post-mastectomy radiation is typically recommended if:
- The tumor exceeds 5 centimeters
- Cancer has spread to lymph nodes
Radiation reduces recurrence near the original tumor site and may enhance survival chances, especially in early-stage breast cancer cases. Side effects can include skin redness, swelling, fatigue, and, in rare cases, rib fractures or mild lung inflammation.
Chemotherapy and Hormone Blockers
Chemotherapy and hormone blockers (such as tamoxifen or aromatase inhibitors) are standard treatments to inhibit cancer spread. Factors like lymph node involvement, menopausal status, hormone receptor presence, and genetic markers (e.g., HER2) influence chemotherapy decisions.
For hormone-sensitive cancers, hormone blockers can be as effective as chemotherapy. Tamoxifen, which blocks estrogen receptors, is often prescribed for five to ten years to increase survival. Aromatase inhibitors, which lower estrogen levels, are an option for postmenopausal women but may increase osteoporosis risk.
HER2-Directed Therapy
HER2-targeted treatments, such as trastuzumab and pertuzumab, may benefit patients whose cancers have excess HER2 receptors. These drugs inhibit cancer cell growth and are often combined with chemotherapy. Monitoring for heart health is necessary, as these medications can weaken the heart.
Managing Noninvasive and Early-Stage Breast Cancer
For ductal carcinoma in situ (DCIS), treatment usually involves either a mastectomy or lumpectomy, possibly followed by radiation therapy. If hormone receptors are present, hormone blockers may also be prescribed.
Lobular carcinoma in situ (LCIS) is not cancerous but increases future cancer risk. Options for LCIS include close monitoring and sometimes tamoxifen or other hormone blockers to reduce cancer risk. Bilateral mastectomy might be considered for high-risk cases.
Treatment Options for Advanced Breast Cancer (Stage III and IV)
For locally advanced breast cancer, treatment typically starts with chemotherapy to shrink the tumor before surgery. Surgery might be followed by radiation, chemotherapy, hormone blockers, or a combination, depending on tumor size, lymph node involvement, and hormone receptor presence.
In cases of metastatic breast cancer (Stage IV), treatment can relieve symptoms and improve life quality, even if it can’t cure the cancer. Decisions about treatment often depend on the patient’s preferences, quality of life considerations, and response to therapies.
Treatment for Specific Breast Cancer Types
- Inflammatory Breast Cancer: Treatment includes chemotherapy, radiation, and typically mastectomy.
- Paget Disease of the Breast: Often treated with mastectomy or breast-conserving surgery plus lymph node removal, usually followed by radiation.
- Phyllodes Tumors: These tumors require removal with a wide margin of surrounding tissue. If large, a simple mastectomy may be performed. Recurrence risks depend on the margin width and whether the tumor is cancerous.
Fertility Preservation
Women undergoing breast cancer treatment should avoid pregnancy. For those wishing to preserve fertility, consultation with a reproductive endocrinologist before treatment is essential to discuss options like ovarian stimulation and egg or embryo freezing. The choice of preservation technique depends on the breast cancer type, planned treatments, and patient preference.
Follow-up Care
After initial treatment, regular follow-up exams, including physical assessments and mammograms, are essential. Self-exams and monitoring for symptoms—such as new lumps, pain, nipple changes, loss of appetite, unexplained cough, or neurological symptoms—are advised. Routine diagnostic tests are not necessary unless symptoms suggest recurrence.
Prognosis and Survival Rates
Survival rates depend on factors like tumor size, cancer type, and lymph node involvement. According to the National Cancer Institute’s SEER Program, the 5-year survival rates are approximately:
- 99% for localized cancer
- 86% for regional spread (nearby lymph nodes)
- 29% for distant metastasis
Factors for a Poorer Prognosis
- Younger diagnosis age (20s or 30s)
- Larger, rapidly-dividing tumors lacking well-defined borders
- Tumors without estrogen/progesterone receptors
- Excessive HER2 receptors
- BRCA1 gene mutation
Women with a BRCA2 mutation don’t face worse outcomes from their initial cancer but do have higher risks for developing a second cancer.
End-of-Life Considerations
In metastatic breast cancer, quality of life may take precedence over prolonged life, with symptom management focused on comfort. Pain and other symptoms, such as nausea or difficulty breathing, can be managed with medications. Psychological and spiritual support, as well as counseling, are available to help patients cope.
Advance directives for treatment preferences and updating wills are recommended for women with metastatic breast cancer, ensuring that their wishes are known in case they cannot make future decisions.
Frequently Asked Questions (FAQs)
What are the early signs of breast cancer?
Early signs may include a painless lump, breast changes, and nipple discharge. Regular screenings are crucial for early detection.
Is breast cancer hereditary?
Some breast cancers are linked to inherited genetic mutations, such as BRCA1 and BRCA2. However, most cases are not directly inherited.
Can men get breast cancer?
Yes, although rare, men can develop breast cancer and should report any unusual symptoms to their doctor.
What does a breast cancer lump feel like?
A breast cancer lump often feels firm, irregular, and is usually painless. However, not all lumps are cancerous.
How often should I get a mammogram?
For women aged 50 to 74, mammograms are generally recommended every two years. Women at higher risk may need more frequent screenings.
Conclusion
Understanding breast cancer’s symptoms, types, risk factors, and treatments is essential for early detection and effective treatment. Awareness of personal risk factors, including family history, lifestyle choices, and regular screenings, can help individuals stay proactive about breast health. If diagnosed, a range of effective treatment options are available, tailored to each case.
Breast cancer awareness and regular screenings are critical. Knowledge empowers individuals to recognize early symptoms, seek timely medical advice, and make informed decisions regarding treatment options.