Bacterial Vaginosis vs Yeast Infection: Key Differences, Treatment & Prevention
Itching, burning, and irritation in the vaginal area can often lead to confusion regarding the exact cause of the symptoms. While many may assume a yeast infection, a lesser-known yet common condition called bacterial vaginosis (BV) could be the culprit. Understanding the difference between these two common infections is crucial for receiving the correct treatment and avoiding prolonged discomfort. In this article, we will explore the causes, symptoms, and treatments of both bacterial vaginosis and yeast infections, helping readers to distinguish between them and seek appropriate care.
What is Bacterial Vaginosis (BV)?
Bacterial vaginosis (BV) is the most common cause of vaginal infections and arises from an imbalance in the natural flora of the vagina. This imbalance often occurs when the protective, peroxide-producing lactobacilli (good bacteria) are diminished, allowing for the overgrowth of anaerobic bacteria and other harmful pathogens, such as Gardnerella vaginalis and Mycoplasma hominis. Approximately 50% of all vaginal infections are classified as BV, while only 25% are attributed to yeast infections.
Symptoms of BV can include:
- An abnormal vaginal discharge that may appear thin, white, or gray with a distinct, unpleasant fishy odor, especially noticeable after sex or during menstruation.
- Vaginal itching.
- A burning sensation during urination.
- Vaginal discomfort.
Although BV is usually not dangerous and can often go unnoticed—approximately half of women with BV experience no noticeable symptoms—when symptoms do appear, they can be quite distressing. It’s crucial to understand that attempting to mask the symptoms with sprays, gels, or perfumed soaps is ineffective and can potentially worsen the condition. The only real solution is to restore and maintain the delicate balance of the vaginal flora.
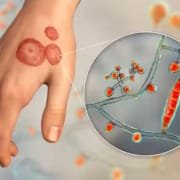
What is a Yeast Infection?
A yeast infection is a type of vaginitis caused by the overgrowth of yeast, primarily a fungus known as Candida, which is naturally present in the body. Yeast infections can occur for various reasons, including a compromised immune system, hormonal changes, increased sexual activity, or pregnancy. While yeast infections are not classified as sexually transmitted infections (STIs), sexual activity can contribute to their development by causing small breaks in the skin that allow yeast to proliferate.
Statistics indicate that about 75% of women will experience a yeast infection at some point in their lives, and many will have multiple occurrences. The symptoms of a yeast infection can closely resemble those of BV but typically include:
- Vaginal itching and irritation, particularly of the vulva.
- Pain or soreness.
- Thick, white vaginal discharge that is odor-free and resembles cottage cheese.
- A burning sensation during urination or sexual intercourse.
- Redness and swelling of the vulva.
It is important to note that while both BV and yeast infections cause discomfort and changes in vaginal discharge, they have distinct underlying causes. In some cases, women may experience recurrent yeast infections or BV, which can be frustrating and require further medical evaluation.
Causes of BV and Yeast Infections
While BV and yeast infections share similarities in symptoms, their causes differ significantly. BV is typically triggered by disruptions to the vaginal flora’s natural balance. In a healthy state, the beneficial bacteria (lactobacilli) outnumber the harmful bacteria. However, various factors can disrupt this balance and lead to BV, including:
- Douching or excessive vaginal cleansing, which can wash away the healthy bacteria.
- Hormonal fluctuations associated with menstruation, pregnancy, or menopause, which can alter the vaginal environment.
- Having sexual intercourse with a new partner or with multiple partners, increasing the risk of bacterial exposure.
- Smoking, which has been associated with an increased risk of BV.
- Stress, which can impact the immune system and the body’s ability to maintain a balanced flora.
Yeast infections, on the other hand, are primarily caused by an overgrowth of Candida, which is usually kept in check by lactobacilli. Factors that can lead to this overgrowth include:
- Use of hormonal contraceptives or hormone therapies that increase estrogen levels, providing a more favorable environment for yeast.
- Recent antibiotic use that disrupts the natural bacterial balance, allowing yeast to proliferate unchecked.
- Uncontrolled diabetes, as high blood sugar levels can promote yeast growth.
- Pregnancy, during which hormonal changes can alter the vaginal environment.
- A weakened immune system due to conditions such as HIV/AIDS, cancer treatments, or certain medications.
Both BV and yeast infections are not considered STIs, although they can develop as a result of sexual activity. Understanding the causes of these infections can help in adopting preventive measures and reducing risk factors.
Differences Between BV and Yeast Infections
Bacterial vaginosis and yeast infections can both result in vaginitis, which is characterized by inflammation of the vagina. Vaginitis can lead to uncomfortable symptoms, including itching, pain, burning, changes in vaginal discharge, and foul-smelling odor. When diagnosing the cause of vaginitis, healthcare professionals typically identify BV in approximately 40-50% of cases and yeast infections in 20-25% of cases.
Here is a table summarizing the differences in symptoms between BV and yeast infections:
| Symptoms | Bacterial Vaginosis (BV) | Yeast Infection |
|---|---|---|
| Vaginal Discharge | Thin, gray or white, with a fishy odor. | Thick, white, cottage cheese-like, odor-free. |
| Odor | Strong, unpleasant, “fishy” odor. | No odor. |
| Discomfort | Vaginal discomfort without inflammation. | Pain or discomfort, often with inflammation. |
| Burning Sensation | Burning sensation when urinating. | Burning sensation during intercourse or urination. |
| Vaginal Itching | Vaginal itching may occur. | Intense vaginal itching. |
| Vulvar Redness | No redness or inflammation of the vulva. | Redness and inflammation of the vulva. |

Diagnosis
Determining whether a vaginal infection is due to BV or a yeast infection typically involves a visit to a healthcare professional. The diagnosis process may include:
- A thorough medical history review, including any previous vaginal infections and treatments.
- A physical examination to check for signs of infection and assess vaginal discharge.
- Sampling of vaginal discharge for laboratory analysis to identify harmful bacteria or fungi.
- Testing the vaginal pH, as a pH level of 4.5 or higher may indicate BV.
It is worth noting that about 20% of healthy women may have Candida in their vaginas without any symptoms, so a positive fungal culture does not necessarily mean the fungus is responsible for symptoms.
Treatment
The treatments for BV and yeast infections differ, and the appropriate treatment will depend on the severity of the infection.
BV Treatment
To treat bacterial vaginosis, a healthcare provider may prescribe antibiotics, including:
- Metronidazole (Flagyl): Available as a pill or vaginal gel, often taken for five to seven days.
- Clindamycin (Cleocin): A cream that is inserted into the vagina, usually applied at bedtime for seven days.
- Tinidazole (Tindamax): Available in pill form, typically taken as a single dose or over a course of days.
Yeast Infection Treatment
For mild to moderate symptoms of a yeast infection, healthcare providers may recommend antifungal medications, such as:
- Fluconazole (Diflucan): An oral antifungal medication taken as a single dose, effective for most cases.
- Over-the-counter antifungal creams or suppositories: Products containing clotrimazole, miconazole, or tioconazole can be used for seven days for relief from symptoms.
It is crucial to complete the entire course of medication, even if symptoms improve before treatment is finished. This helps ensure that the infection is entirely eradicated and prevents a recurrence.
Preventive Measures
Preventing bacterial vaginosis and yeast infections involves adopting healthy hygiene practices and lifestyle changes. Here are some recommendations:
- Maintain Proper Hygiene: Practice good vaginal hygiene by washing the external genital area with mild soap and water. Avoid using harsh soaps, douches, and perfumed products that can irritate the vaginal area.
- Wear Breathable Underwear: Choose cotton underwear that allows for air circulation and moisture control, as this can help prevent the growth of yeast.
- Limit Antibiotic Use: Only take antibiotics when necessary, as they can disrupt the natural balance of bacteria in the vagina.
- Manage Diabetes: Keeping blood sugar levels in check can reduce the risk of developing yeast infections.
- Consider Probiotics: Probiotic supplements or yogurt containing live cultures may help maintain a healthy balance of vaginal flora.
- Practice Safe Sex: While BV is not considered an STI, using condoms can help reduce the risk of irritation and infections during sexual activity.
- Limit Sexual Partners: Having fewer sexual partners can help reduce the risk of developing BV.
When to Seek Medical Attention
If you experience symptoms such as unusual vaginal discharge, burning sensations, or persistent itching, it is advisable to consult a healthcare provider. Early diagnosis and treatment can prevent complications and ensure proper management of both bacterial vaginosis and yeast infections. Additionally, if you have a history of recurrent infections or if over-the-counter treatments are ineffective, it is essential to seek medical advice to explore underlying causes and receive appropriate treatment.
Frequently Asked Questions (FAQs)
How does discharge differ between bacterial vaginosis (BV) and a yeast infection?
Bacterial vaginosis (BV) causes thin, gray or white discharge with a fishy odor, while a yeast infection leads to thick, white, odorless discharge.
How do urinary tract infections (UTIs) compare with bacterial vaginosis (BV) and yeast infections?
UTIs often cause painful urination and abdominal discomfort, whereas bacterial vaginosis (BV) and yeast infections primarily lead to vaginal symptoms like odor and discharge.
How does trichomoniasis differ from bacterial vaginosis (BV) and yeast infections?
Trichomoniasis is a sexually transmitted infection that can cause greenish discharge and is often associated with discomfort during intercourse, unlike bacterial vaginosis (BV) and yeast infections.
What is the difference between bacterial vaginosis (BV) and a yeast infection?
Bacterial vaginosis (BV) is caused by an imbalance of bacteria, while a yeast infection is caused by an overgrowth of Candida yeast. Symptoms and treatments differ significantly.
How do treatment options differ between bacterial vaginosis (BV) and a yeast infection?
Treatment for bacterial vaginosis (BV) typically involves antibiotics, while antifungal medications are used for yeast infections. Self-treatment is not recommended without a proper diagnosis.
What is the smell associated with bacterial vaginosis (BV) vs. a yeast infection?
Bacterial vaginosis (BV) is characterized by a strong, fishy odor, especially after intercourse, while a yeast infection typically has no significant odor.
How do bacterial vaginosis (BV), yeast infections, and trichomoniasis compare?
All three are types of vaginitis with differing causes and symptoms. Bacterial vaginosis (BV) is due to bacterial imbalance, yeast infections are caused by Candida overgrowth, and trichomoniasis is a sexually transmitted infection.
Conclusion
Bacterial vaginosis and yeast infections are common conditions that can cause discomfort and anxiety among women. Understanding the differences in symptoms, causes, and treatments can empower women to seek the appropriate care and find relief. Taking preventive measures can significantly reduce the risk of both infections, and being aware of one’s body and its signals is essential for maintaining overall reproductive health. If you suspect you have either condition, don’t hesitate to reach out to a healthcare provider for guidance and support. Remember that early intervention is key to effective management and relief from symptoms.