Bacterial Vaginosis: Causes, Symptoms, and Treatments
Bacterial vaginosis (BV) is a common vaginal condition caused by an imbalance in the normal bacteria that reside in the vagina. This condition is characterized by an overgrowth of certain bacteria, leading to a range of symptoms, most notably an unusual vaginal discharge with a fishy odor. BV is not an infection but rather a disruption in the natural balance of the vaginal flora. Understanding bacterial vaginosis is essential for effective management and prevention. This comprehensive guide covers the causes, symptoms, and treatments for bacterial vaginosis, offering valuable insights for individuals affected by or concerned about this condition.
What is Bacterial Vaginosis?
Bacterial vaginosis occurs when the delicate balance of bacteria in the vagina is disrupted. Normally, the vagina is home to various bacteria, with Lactobacillus species being predominant. In BV, there is a decrease in these Lactobacillus bacteria and an increase in anaerobic bacteria, leading to symptoms such as an abnormal discharge and a fishy odor. While bacterial vaginosis can affect anyone with a vagina, it is important to note that it is not classified as a sexually transmitted infection (STI) because it arises from an imbalance of normally present bacteria rather than from an external source.
Key Facts About Bacterial Vaginosis
Bacterial vaginosis (BV) is the leading cause of abnormal vaginal discharge among women of reproductive age.
The prevalence of BV varies by region and population, with recent global estimates showing that between 23% and 29% of women in this age group are affected.
BV predominantly affects sexually active women, with higher incidence linked to inconsistent condom use and having multiple or new sexual partners.
BV can increase the risk of acquiring HIV and other sexually transmitted infections (STIs). Additionally, if left untreated, BV may lead to complications during pregnancy, including potential adverse effects.
Causes of Bacterial Vaginosis
The exact cause of bacterial vaginosis is not fully understood. However, certain factors can disrupt the natural balance of bacteria in the vagina, increasing the likelihood of developing BV. These factors include.
- Bacterial Imbalance. BV typically results from a reduction in Lactobacillus bacteria and an overgrowth of other bacteria, such as Gardnerella vaginalis and various anaerobes.
- Sexual Activity. Although BV is not classified as an STI, sexual activity can influence the vaginal bacterial balance. The condition is more common in individuals with multiple sexual partners and those who engage in sexual activity with a female partner.
- Hygiene Practices. Frequent douching, the use of scented vaginal products, and excessive washing can disrupt the natural vaginal environment and increase the risk of BV.
- Other Factors. Smoking, high-stress levels, and a history of bacterial vaginosis can also contribute to the development of this condition.
- Hormonal Changes. Using an intrauterine device (IUD) for contraception may also be a factor.
Although BV is not an STI, it can be triggered by sexual activity. It’s also important to note that BV can be transmitted between women during sexual contact.
Symptoms of Bacterial Vaginosis
The symptoms of BV can vary, and some women may not experience any symptoms at all. When symptoms do occur, they often include.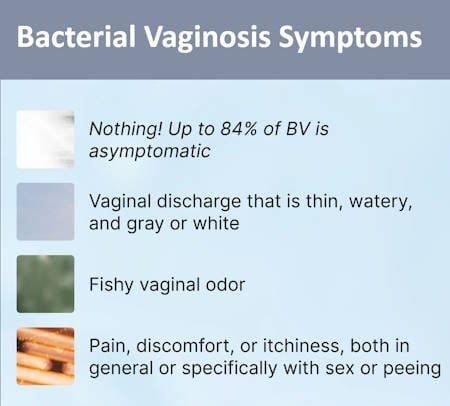
- Abnormal Discharge. The most noticeable symptom is a thin, gray or white discharge that often has a fishy odor. This odor may become more prominent after sexual intercourse.
- Odor. A fishy smell is a common characteristic of BV, though not everyone with BV will experience this.
- Lack of Discomfort. BV typically does not cause itching or soreness. If you are experiencing these symptoms, another condition might be present.
- Vaginal Irritation. Some individuals may experience mild itching or irritation in the vaginal area, although many women with BV are asymptomatic.
- Burning Sensation. A burning sensation during urination or sexual intercourse can occur in some cases.
It’s important to note that many women with BV do not have noticeable symptoms. If you are experiencing unusual vaginal discharge, it is crucial to consider other potential causes and consult with a healthcare provider for an accurate diagnosis.
Diagnosis of Bacterial Vaginosis
Diagnosing bacterial vaginosis involves a combination of clinical evaluation and laboratory tests.
- Medical History. A healthcare provider will inquire about symptoms, sexual history, hygiene practices, and any previous occurrences of BV.
- Pelvic Examination. A pelvic exam is conducted to assess the characteristics of the vaginal discharge and to exclude other conditions such as yeast infections or sexually transmitted infections.
- Microscopic Examination. A sample of vaginal discharge is examined under a microscope to identify the presence of “clue cells”—vaginal epithelial cells that have a stippled appearance due to being coated with bacteria.
- pH Testing. The vaginal pH is measured using pH paper. An elevated pH (greater than 4.5) can indicate BV.
- Whiff Test. Adding potassium hydroxide (KOH) to the vaginal discharge sample may release a characteristic fishy odor, which is indicative of BV.
- Amsel Criteria. The Amsel criteria require the presence of at least three out of four indicators—thin gray discharge, clue cells on microscopy, elevated vaginal pH, and a fishy odor after adding KOH.
Treatment Options for Bacterial Vaginosis
Bacterial vaginosis often resolves without treatment, but medical intervention is recommended for symptomatic individuals or those with recurrent episodes. Treatment options include.
- Antibiotic Therapy.
- Metronidazole. Available as oral tablets (500 mg twice daily for 7 days) or a gel (0.75% applied intravaginally once daily for 5 days).
- Clindamycin. Available as a cream (2% applied intravaginally nightly for 7 days) or a single-dose gel (2% applied intravaginally).
- Alternative Treatments.
- Tinidazole. An oral antibiotic that can be taken daily for 5 days or as a higher dose for 2 days.
- Secnidazole. Approved by the FDA as a single-dose oral granule treatment for BV.
- Probiotics. Although evidence is not conclusive, some studies suggest that probiotics containing Lactobacillus may help reduce recurrence rates.
- Boric Acid. Used intravaginally, it may be recommended for recurrent BV, though it is not FDA-approved for this purpose.
Prevention and Management of Bacterial Vaginosis
To reduce the risk of developing bacterial vaginosis, consider the following.
- Avoid Douching. Douching disrupts the natural vaginal flora and can increase the risk of BV.
- Use of Condoms. Consistent use of condoms during sexual activity can help maintain a healthy vaginal environment.
- Regular Gynecological Exams. Regular check-ups can help detect and manage bacterial vaginosis early.
- Healthy Hygiene Practices. Avoiding scented vaginal products and using mild soap can help maintain vaginal health.
- Wipe from front to back after using the toilet to minimize the spread of bacteria.
- Change menstrual products regularly to maintain hygiene.
- Choose breathable, loose-fitting underwear made from natural fabrics and change it frequently.
If you experience symptoms of BV, here are some steps to alleviate discomfort.
- Shower Instead of Bathing. Baths can sometimes aggravate symptoms.
- Avoid Vaginal Deodorants. Use regular soap and water to clean the genital area.
- Wear Cotton Underwear. Cotton allows for better airflow and can help keep the vaginal area dry.
Complications of Bacterial Vaginosis
If left untreated, bacterial vaginosis can lead to several complications, including.
- Increased Risk of STIs. BV can increase susceptibility to sexually transmitted infections, including HIV and herpes.
- Pregnancy Complications. Pregnant individuals with BV may face an increased risk of preterm birth, premature rupture of membranes, and postpartum infections.
- Pelvic Inflammatory Disease (PID). BV can contribute to the development of PID, which may lead to infertility if not addressed.
Bacterial Vaginosis and Pregnancy
If you develop bacterial vaginosis during pregnancy, there is a small risk of complications such as premature birth or miscarriage. However, most pregnancies with BV proceed without issues. If you notice any changes in your vaginal discharge during pregnancy, consult your healthcare provider or midwife for guidance.
Bacterial Vaginosis vs. Yeast Infection
Bacterial vaginosis and yeast infections (vulvovaginal candidiasis) can have similar symptoms, such as vaginal discharge and discomfort. However, they are distinct conditions with different causes and treatments.
- Cause. BV is primarily caused by an imbalance in vaginal bacteria, while yeast infections are caused by an overgrowth of the fungus Candida.
- Discharge. BV discharge is thin and watery with a fishy odor, whereas yeast infection discharge is typically thick and white, resembling cottage cheese.
- Odor. BV is associated with a fishy odor, while yeast infections usually do not have a strong odor.
Accurate diagnosis is crucial because treatments for these conditions differ. Yeast infections can often be treated with over-the-counter antifungal medications, while BV usually requires prescription antibiotics. For more details about vaginal yeast infection read “Vaginal Yeast Infections: Symptoms, Causes and Treatment“.
Recurrent Bacterial Vaginosis
Recurrent bacterial vaginosis (BV) is a common issue, as it often resists treatment or reoccurs even after successful therapy.
One reason for this persistence could be the formation of a biofilm in your vaginal microbiome. Bacteria, always striving to survive, can create biofilms—protective layers that shield them from external threats. Biofilms make bacteria more resilient and harder to eliminate, which can render treatments like antibiotics less effective. This may contribute to the high recurrence rate of BV, although research is still ongoing to fully understand the role of biofilms in BV.
To help prevent BV from recurring, consider incorporating probiotics into your routine. Probiotics with beneficial strains of vaginal bacteria can reinforce your natural defenses against harmful pathogens, even when you’re undergoing antibiotic treatment.
In addition to medication, adopting some preventive measures can help reduce the likelihood of BV coming back
Frequently Asked Questions (FAQs)
- Can you get BV without having sex?Yes, bacterial vaginosis can occur even if you’re not sexually active, which is why it isn’t classified as a sexually transmitted infection (STI). While sex can be a contributing factor, other triggers such as menstruation, smoking, and douching can also increase the risk of developing BV.
- Will BV go away on its own?BV may sometimes resolve on its own, particularly if it doesn’t cause symptoms. Your immune system might clear the infection before you even notice it. However, it’s advisable to consult with a healthcare provider if you experience symptoms of BV. Untreated BV can elevate the risk of sexually transmitted infections, pelvic inflammatory disease, and infertility.
- Is BV a yeast infection?No, bacterial vaginosis and yeast infections are distinct conditions. BV results from an imbalance in vaginal bacteria, leading to a fishy odor and thin, gray discharge. In contrast, yeast infections are caused by an overgrowth of the Candida fungus, which results in thick, white discharge along with itching and burning. BV is typically treated with antibiotics, whereas yeast infections are treated with antifungal medications. Understanding these differences is crucial for proper diagnosis and treatment.
- Can bacterial vaginosis be treated at home?
While some home remedies may help alleviate symptoms, it is crucial to seek professional medical treatment for a proper diagnosis and effective management. - Is bacterial vaginosis an STI?
No, Bacterial vaginosis is not classified as a sexually transmitted disease (STD). It is not caused by a single pathogen and does not typically affect men. However, it can be more prevalent among sexually active women and can increase the risk of acquiring STDs due to changes in the vaginal environment.. - How long does it take for treatment to work?
Antibiotic treatments typically lead to symptom relief within a week. However, some individuals may experience recurrence and may need additional treatment. - Can bacterial vaginosis recur after treatment?
Yes, bacterial vaginosis can recur in some individuals. Up to 80% of women may experience a recurrence within 9 months of treatment. - Is it necessary to treat my sexual partner for bacterial vaginosis?
Since BV is not an STI, partners do not need to be treated. There is no risk of passing the condition back and forth between partners.
Conclusion
By understanding bacterial vaginosis, its causes, symptoms, and treatment options, individuals can take proactive steps to manage and prevent this common condition. Regular gynecological care and maintaining healthy hygiene practices are essential for maintaining vaginal health and overall well-being.
For further information, or if you have concerns about bacterial vaginosis or any other health issues, consult with a healthcare professional. They can provide personalized advice and treatment options based on your specific needs.