Angular Cheilitis: What It Is, Symptoms, Causes & Treatment
What Is Angular Cheilitis?
Angular cheilitis is a condition characterized by inflamed, cracked, and often painful sores at the corners of the mouth. These sores in the corner of the mouth can range from mild redness to deep, bleeding fissures. The condition is often caused by a combination of factors, including excess saliva accumulation, fungal or bacterial infections, and underlying health issues like iron or vitamin deficiencies. While it can be uncomfortable, angular cheilitis is typically treatable with proper care and medication.
Symptoms of Angular Cheilitis
The symptoms of angular cheilitis are usually localized to the corners of the mouth. If you’re experiencing this condition, you may notice:
- Bleeding at the corners of the mouth
- Redness and swelling
- Cracked mouth corners or deep fissures
- Blisters or crusty patches
- Itching or burning sensations
- Pain when opening the mouth or eating
In some cases, angular cheilitis may also be accompanied by other symptoms, such as:
- Oral yeast infections (thrush)
- An eczema-like rash on the lower face
- Redness on the roof of the mouth, especially in denture wearers
- Excess saliva pooling at the corners of the mouth
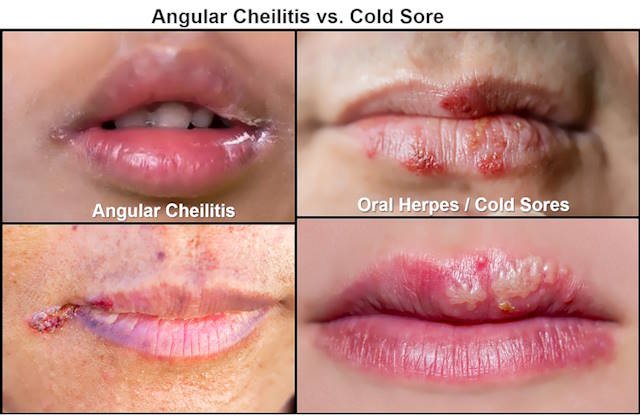
Angular Cheilitis vs. Cold Sores
Many people confuse angular cheilitis with cold sores, but the two conditions are quite different. While cold sores are caused by the herpes simplex virus and can appear anywhere on the lips, angular cheilitis specifically affects the corners of the mouth. Cold sores often start as itchy or painful spots that develop into blisters, while angular cheilitis begins as dry, irritated skin that can progress to swollen, cracked patches.
Another key difference is that cold sores are contagious, while angular cheilitis is not. If you’re unsure whether you’re dealing with angular cheilitis or a cold sore, consult a healthcare provider for an accurate diagnosis.
What Causes Angular Cheilitis?
Angular cheilitis occurs when saliva accumulates in the corners of the mouth, leading to dryness and cracking. Once the skin is cracked, it becomes susceptible to infections caused by yeast (like Candida) or bacteria (such as Staphylococcus). Several factors can contribute to this condition, including:
- Ill-fitting dentures or dental appliances that cause skin folds at the corners of the mouth
- Nutritional deficiencies, particularly iron, riboflavin (vitamin B2), or cobalamin (vitamin B12)
- Fungal or bacterial infections that thrive in moist environments
- Atopic dermatitis or eczema, which can make the skin more prone to irritation
- Drooling during sleep, which keeps the corners of the mouth moist
- Misaligned teeth or jaw structure that creates skin folds
- Prolonged use of face masks, which can trap moisture and irritate the skin
Understanding the underlying cause of your angular cheilitis is crucial for effective treatment. For example, if the condition is caused by a fungal infection, an angular cheilitis cream containing antifungal medication may be prescribed. If nutritional deficiencies are to blame, supplements or dietary changes may be recommended.
How Common Is Angular Cheilitis?
Angular cheilitis affects approximately 0.7% of the general population in the United States. However, certain groups are more prone to developing this condition. It is the most common bacterial or fungal infection of the lips and tends to occur more frequently in children and adults aged 30 to 60. Among the elderly, the prevalence rises to about 11%, with denture wearers being three times more likely to develop angular cheilitis. Men are also twice as likely to experience this condition, often due to factors like denture use and underlying health issues.
Certain medical conditions can increase the risk of angular cheilitis. For example, up to 10% of individuals with HIV may develop oral thrush, which can accompany angular cheilitis. Similarly, patients with inflammatory bowel disease (IBD), such as Crohn’s disease or ulcerative colitis, have a higher likelihood of developing this condition. In rare cases, like orofacial granulomatosis, the incidence of angular cheilitis can be as high as 20%.
Risk Factors for Angular Cheilitis
While anyone can develop angular cheilitis, certain factors can increase your risk. These include:
- Poor-fitting dentures or dental appliances
- Misaligned teeth that create skin folds at the corners of the mouth
- Significant weight loss, which can alter facial structure
- Frequent lip licking, which keeps the area moist and prone to cracking
- Smoking, which can irritate the skin
- Nutritional deficiencies, particularly in B vitamins like riboflavin and cobalamin
- Frequent antibiotic use, which can disrupt the balance of bacteria and fungi
- Use of retinoid products, which can dry out the skin
- Weakened immune system due to conditions like HIV or diabetes
- Age over 75, as skin becomes thinner and more prone to irritation
- Dry mouth, which can exacerbate cracking
- Inflammatory disorders like Sjögren’s syndrome
- Chronic health conditions such as diabetes or inflammatory bowel disease (IBD)
- Down syndrome, which is associated with a higher risk of oral health issues
How Is Angular Cheilitis Diagnosed?
If you suspect you have angular cheilitis, a doctor or dermatologist can diagnose the condition. During the examination, they will inspect the corners of your mouth for signs of redness, cracking, or swelling. They may also ask about your medical history, medications, and lifestyle to identify potential causes.
In some cases, your doctor may take a culture swab from the affected area to test for fungal or bacterial infections. This step is usually reserved for cases where initial treatments have not been effective.
How Is Angular Cheilitis Treated?
The treatment for angular cheilitis depends on its underlying cause. Here are some common approaches:
1. Nutritional Deficiencies
If a lack of essential nutrients like iron or B vitamins is causing your angular cheilitis, your doctor may recommend dietary changes or supplements to address the deficiency.
2. Fungal Infections
For angular cheilitis caused by a yeast infection, an angular cheilitis cream containing antifungal medication, such as clotrimazole, may be prescribed.
3. Bacterial Infections
If bacteria are the culprit, your doctor may recommend a topical antibiotic ointment, such as mupirocin, to clear the infection.
4. Other Treatment Options
Additional treatments may include:
- Topical antiseptics to keep the sores clean and prevent infection
- Topical steroid ointments to reduce inflammation and discomfort
- Filler injections to reduce skin folds at the corners of the mouth
5. Managing Dry Mouth
If dry mouth is contributing to your angular cheilitis, try these tips:
- Chew sugar-free gum to stimulate saliva production
- Suck on sugar-free candies or lozenges
- Use a humidifier at home to add moisture to the air
- Stay hydrated by drinking water throughout the day
When to See a Doctor
If home remedies like petroleum jelly don’t improve your symptoms or if your angular cheilitis worsens, it’s important to consult a doctor. Untreated angular cheilitis can lead to persistent infections or other complications. Additionally, if you experience recurring episodes of angular cheilitis alongside other symptoms, a medical evaluation can help identify underlying health issues.
Can Angular Cheilitis Cause Complications?
While most cases of angular cheilitis are straightforward to treat, complications can arise if the condition is left untreated. If the underlying cause is a bacterial or fungal infection, the infection may spread to nearby skin or lead to oral thrush. This is why it’s important to address the root cause of angular cheilitis promptly. Proper treatment, such as using an angular cheilitis cream or medication, can prevent these complications and promote healing.
Is Angular Cheilitis Contagious?
Angular cheilitis is not contagious in most cases. Unlike cold sores, which are caused by the herpes virus and can spread through contact, angular cheilitis is typically caused by factors like saliva buildup, fungal or bacterial infections, or nutritional deficiencies. However, if bacteria or yeast grow in the cracked skin over time, it’s still a good idea to avoid sharing utensils or personal items until the condition is treated.
If you’re unsure whether your mouth sores are angular cheilitis or cold sores, consult a healthcare provider for an accurate diagnosis. This will help you take the right steps to manage the condition and avoid spreading it to others.
How to Prevent Angular Cheilitis
Preventing angular cheilitis involves maintaining good hygiene and keeping the skin around your mouth healthy. Here are some practical tips to reduce your risk:
- Keep the Skin Moisturized: Dry, cracked skin is more prone to irritation and infection. Apply a protective barrier, such as petroleum jelly or coconut oil, to the corners of your mouth to lock in moisture and prevent saliva from accumulating.
- Use Lip Balm Regularly: Regularly applying lip balm can help prevent chapped lips and reduce the risk of angular cheilitis. Look for products with moisturizing ingredients like beeswax or shea butter.
- Prevent Dry Mouth: Dry mouth can lead to increased saliva production, contributing to angular cheilitis. To manage this, chew sugar-free gum to stimulate saliva flow, use a humidifier to add moisture to the air, and stay hydrated by drinking plenty of water.
- Address Underlying Causes: If the structure of your mouth or facial creases contributes to angular cheilitis, talk to your doctor about solutions like oral appliances or fillers. Additionally, addressing nutritional deficiencies or treating underlying health conditions can help prevent recurrence.
Key Takeaways
Angular cheilitis is a common inflammatory condition that causes redness, cracking, and sores at the corners of the mouth. While it’s usually not serious, it can be uncomfortable and may lead to complications if left untreated. The good news is that angular cheilitis typically responds well to treatment once the underlying cause is identified.
If your symptoms don’t improve within two weeks, worsen, or recur frequently, it’s important to consult a doctor. They can help determine the cause and recommend appropriate treatments, such as angular cheilitis medication, antifungal creams, or dietary changes.
By practicing good hygiene, keeping your skin moisturized, and addressing any underlying health issues, you can reduce your risk of developing angular cheilitis and maintain healthy, comfortable lips.
Frequently Asked Questions About Angular Cheilitis
Is there an overnight cure for angular cheilitis?
While there’s no guaranteed angular cheilitis overnight cure, some treatments can provide quick relief. Applying a thick layer of petroleum jelly or an antifungal cream before bed can help reduce dryness and promote healing overnight. However, addressing the underlying cause, such as a fungal infection or nutritional deficiency, is essential for long-term improvement.
Can angular cheilitis be caused by cold sores?
No, angular cheilitis and cold sores are different conditions. Angular cheilitis is caused by factors like fungal or bacterial infections, saliva buildup, or nutritional deficiencies, while cold sores are caused by the herpes simplex virus. If you’re unsure whether you have angular cheilitis vs cold sore, consult a healthcare provider for an accurate diagnosis.
What’s the difference between angular cheilitis and a lip split in the corner?
A lip split in the corner is often a symptom of angular cheilitis. The condition causes the corners of the mouth to crack, bleed, and become inflamed. While a lip split can occur due to dryness or irritation, angular cheilitis is typically linked to infections or underlying health issues.
Can I use over-the-counter creams for angular cheilitis?
Yes, over-the-counter antifungal creams or angular cheilitis creams can be effective for mild cases caused by fungal infections. Look for products containing clotrimazole or miconazole. However, if symptoms persist or worsen, consult a doctor for a prescription-strength treatment.
How long does it take for angular cheilitis to heal?
With proper treatment, such as antifungal or antibacterial creams, angular cheilitis can improve within a few days to two weeks. However, healing time depends on the underlying cause and how well you follow the treatment plan. If symptoms persist beyond two weeks, seek medical advice.
Are there natural remedies for angular cheilitis?
Yes, some natural remedies can help manage angular cheilitis. Applying honey, coconut oil, or aloe vera to the affected area can soothe irritation and promote healing. However, these remedies should complement, not replace, medical treatments, especially if the condition is caused by an infection.
Can angular cheilitis affect only one side of the mouth?
Yes, angular cheilitis can affect one or both corners of the mouth. If only one side is affected, it may be due to factors like drooling during sleep or an injury to that specific area. However, if the condition persists, it’s important to determine the underlying cause.
Is angular cheilitis more common in certain seasons?
Angular cheilitis can be more common during colder months when dry air and chapped lips are more prevalent. Using a humidifier and keeping the skin around your mouth moisturized can help prevent flare-ups during winter.
Can stress cause angular cheilitis?
While stress itself doesn’t directly cause angular cheilitis, it can weaken the immune system, making you more susceptible to infections that trigger the condition. Managing stress through relaxation techniques and self-care may help reduce your risk.










