Molluscum Contagiosum: Symptoms, Causes & Treatment
Molluscum Contagiosum is a common viral skin infection caused by the Molluscum Contagiosum Virus (MCV). This infection leads to the development of small, raised, dome-shaped lesions or nodules on the skin, known as mollusca. The infection is generally mild and benign, affecting individuals of all ages, although it is most commonly seen in children. While the condition is not life-threatening, it can cause cosmetic concerns and discomfort for patients.
Molluscum contagiosum, also known as water warts, typically presents with smooth, pink or flesh-colored skin lesions that have a central dimple. Although molluscum contagiosum is usually self-limiting and resolves without treatment, understanding its symptoms, causes, transmission, and treatment options can help in identifying the disease and differentiating it from other serious conditions.
Causes and Transmission
Molluscum contagiosum is caused by the molluscum contagiosum virus (MCV), a poxvirus. This virus has four subtypes (MCV-1 to MCV-4), with MCV-1 being the most common cause of the infection, especially in children. MCV-2 is more commonly seen in adults and individuals with weakened immune systems, such as those with HIV/AIDS. For more details about HIV (Human Immunodeficiency Virus) read “HIV / AIDS: Symptoms, Diagnosis, Treatment, and Prevention”
The virus spreads through direct skin-to-skin contact or indirect contact via contaminated objects such as towels, clothing, or shared swimming pool equipment. It is also considered a sexually transmitted infection (STI) in adults when lesions appear in the genital area. Molluscum contagiosum can spread from one part of the body to another through autoinoculation, a process where an individual transfers the virus from one area of their skin to another, often by scratching.
Common Modes of Transmission:
- Direct skin-to-skin contact
- Sharing personal items (towels, razors, toys)
- Sexual contact (in adults)
- Contaminated surfaces (e.g., swimming pools)
How Common is Molluscum Contagiosum
Molluscum contagiosum affects individuals worldwide, with varying prevalence depending on the region and population. In the United States, molluscum contagiosum accounts for approximately 1% of all skin conditions diagnosed by dermatologists. While this condition is seen in individuals of all ages, it is most prevalent in children under the age of 10 and sexually active adults.
Globally, the virus is more common in tropical regions, where poor hygiene, warm climates, and close living conditions may contribute to its spread. For example, in Mali, molluscum contagiosum is one of the most frequent skin infections among children, while in Australia, nearly 23% of the population tests positive for antibodies against the virus.
Symptoms of Molluscum Contagiosum

Molluscum contagiosum is characterized by the appearance of small, firm, and painless bumps or papules on the skin. These bumps typically have the following features:
- Shape: Dome-shaped with a central dimple (umbilicated)
- Color: Flesh-colored, pink, or pearly
- Size: Usually 1 to 5 millimeters in diameter
- Texture: Smooth and firm
Lesions often appear in clusters and can occur anywhere on the body except the palms and soles. Commonly affected areas include the face, neck, arms, legs, and genital region.
Additional Symptoms:
- Itchiness: Some patients report mild itching around the affected area.
- Redness or inflammation: As lesions begin to heal or are scratched, they may become red or inflamed.
- Secondary infection: Scratching can introduce bacteria, leading to a secondary bacterial infection.
Risk Factors for Molluscum Contagiosum
Several factors can increase the risk of developing molluscum contagiosum:
- Age: Children between the ages of 1 and 10 are most commonly affected.
- Weakened immune system: Individuals with compromised immune systems (e.g., people with HIV/AIDS or those undergoing immunosuppressive therapy) are more prone to the infection.
- Sexual activity: Adults who are sexually active can acquire molluscum contagiosum through skin-to-skin contact in the genital region.
- Living in warm, humid climates: The virus thrives in warmer climates, where close contact between individuals is more likely.
Molluscum Contagiosum Diagnosis
Molluscum contagiosum is primarily diagnosed through clinical examination. A dermatologist can typically identify the infection by observing the characteristic appearance of the lesions. In some cases, dermoscopy (a non-invasive imaging technique) may be used to further assess the bumps. The lesions exhibit a central white or yellow core with peripheral blood vessels under the microscope.
In immunocompromised individuals, where the lesions may present atypically or resemble other conditions such as basal cell carcinoma or cryptococcosis, a biopsy may be performed to confirm the diagnosis.
How Molluscum Contagiosum Spreads in the Body
Once the molluscum contagiosum virus enters the skin, it primarily affects keratinocytes, the outermost cells of the skin. The virus remains confined to the epidermis and does not spread to other parts of the body. It produces proteins that inhibit the body’s immune response, allowing the lesions to persist for several months without triggering significant immune activation.
The virus has an incubation period of 2 weeks to 6 months, meaning that individuals may not show signs of infection immediately after exposure. The infection is usually self-limiting, meaning that it can resolve on its own without medical treatment, although this may take anywhere from 6 to 12 months, or even longer in some cases.
Stages of Molluscum Contagiosum
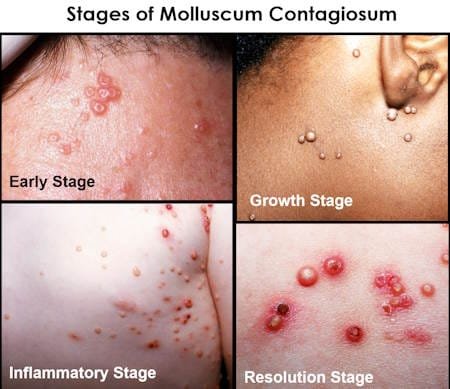
Molluscum contagiosum generally progresses through several stages, although the appearance of these stages may vary slightly depending on individual cases. Here’s a typical outline of the stages.
1. Incubation Period
This is the period after the virus has been contracted but before symptoms appear. The incubation period can last from 2 weeks to 6 months, during which the virus infects the skin cells but does not yet cause visible lesions.
2. Initial Lesion Stage
Small, raised, and smooth papules begin to appear on the skin. These lesions are usually flesh-colored or pink and often have a central dimple or indentation. At this stage, they are typically painless and about 1-5 mm in diameter.
3. Growth Stage
As the infection progresses, the lesions may grow in size, sometimes becoming more prominent. The number of lesions may increase, especially if the virus spreads through skin-to-skin contact or autoinoculation (spreading the virus by scratching or touching affected areas). The lesions may start to take on a waxy or pearly appearance.
4. Inflammatory Stage
In this stage, the body’s immune system begins to react to the virus. Lesions may become red, inflamed, or irritated, which is a sign that the body is fighting off the virus. Itching or discomfort may occur during this stage, and the lesions may be more prone to secondary infections.
5. Resolution Stage
Over time, the immune system successfully eliminates the virus, and the lesions start to heal. They may shrink, flatten, and disappear on their own, leaving behind little to no scarring. This process can take several months to over a year. In people with compromised immune systems, resolution may take longer or require treatment.
Treatment Options for Molluscum Contagiosum
Although molluscum contagiosum is usually self-limiting and resolves without treatment, many individuals seek treatment for cosmetic reasons or to prevent the spread of the infection to others. There are several treatment options available, ranging from physical removal to topical treatments.
1. Physical Removal
- Cryotherapy: Freezing the lesions with liquid nitrogen to destroy the infected tissue.
- Curettage: A surgical technique where lesions are scraped off using a sharp instrument.
- Laser therapy: Pulsed-dye laser or CO2 lasers may be used to remove lesions in certain cases.
These procedures are often painful and may require local anesthesia. Scarring is a potential side effect, and repeated treatments may be necessary.
2. Topical Treatments
Several topical medications can be applied to the affected area to accelerate healing and remove the lesions:
- Imiquimod: A topical cream that stimulates the immune system to attack the virus.
- Cantharidin: A blistering agent applied by a healthcare professional that helps remove the lesions.
- Salicylic acid: A keratolytic agent used to peel off the affected layers of skin.
3. Systemic Treatments
For individuals with a compromised immune system, oral medications such as cimetidine or cidofovir (a DNA polymerase inhibitor) may be used, although they are not typically the first-line treatments. In patients with HIV/AIDS, managing the underlying condition with antiretroviral therapy (ART) can help reduce the severity of molluscum contagiosum.
Complications of Molluscum Contagiosum
While the infection is generally mild, complications can occur, especially in individuals with weakened immune systems:
- Secondary bacterial infection: Scratching the lesions may introduce bacteria, leading to cellulitis or abscess formation.
- Inflammatory dermatitis: Some individuals may develop eczema-like rashes around the lesions.
- Eye complications: If lesions develop near the eyelids, they can cause conjunctivitis.
Prognosis
The prognosis for molluscum contagiosum is typically excellent, as the infection resolves on its own in most cases. However, the duration of the infection can vary, lasting anywhere from 6 months to 5 years. Individuals with weakened immune systems may experience a prolonged course of the disease, and the lesions may be more resistant to treatment.
Prevention of Molluscum Contagiosum
Preventing the spread of molluscum contagiosum involves practicing good hygiene and avoiding direct contact with infected individuals or contaminated objects. To reduce the risk of transmission:
- Avoid sharing personal items such as towels, razors, or clothing.
- Practice safe sex by using condoms and avoiding sexual contact with individuals who have visible lesions.
- Wash hands regularly and maintain good personal hygiene.
- Cover lesions with clothing or bandages to prevent autoinoculation.
Frequently Asked Questions (FAQs)
Is molluscum contagiosum contagious?
Yes, molluscum contagiosum is highly contagious. It spreads through direct skin-to-skin contact or indirect contact with contaminated objects.
Can molluscum contagiosum resolve on its own?
Yes, molluscum contagiosum is usually self-limiting and can resolve on its own within 6 to 12 months. However, treatment may be sought to speed up the process or for cosmetic reasons.
Is molluscum contagiosum an STD?
In adults, molluscum contagiosum can be transmitted sexually, especially when lesions are present in the genital area. However, it can also spread through non-sexual means.
Can molluscum contagiosum leave scars?
Most lesions heal without scarring, but treatments such as cryotherapy or curettage may leave scars, especially if performed improperly.










