HIV / AIDS: Symptoms, Diagnosis, Treatment, and Prevention
HIV (Human Immunodeficiency Virus) is a virus that attacks the body’s immune system, specifically targeting CD4 cells (T cells), which are vital in fighting off infections. If untreated, HIV reduces the number of these cells, making the body more vulnerable to infections and certain cancers. Over time, HIV can lead to the development of AIDS (Acquired Immunodeficiency Syndrome), the most severe phase of HIV infection. Although there is no cure, significant advancements in medical science have made it possible to manage HIV as a chronic condition with proper treatment, allowing individuals to live long and healthy lives. Understanding HIV/AIDS is not only vital for those living with the virus but also for the global community in reducing transmission, improving care, and working towards a future free of HIV/AIDS.
What is HIV and AIDS?
HIV is the virus itself, while AIDS is the final stage of HIV infection, characterized by a severely weakened immune system. Not everyone with HIV will develop AIDS. With appropriate treatment, many people living with HIV can prevent the progression to AIDS.
HIV is primarily transmitted through bodily fluids such as blood, semen, vaginal fluids, rectal fluids, and breast milk. The virus enters the body and begins attacking CD4 cells, which play a critical role in immune defense. Once inside these cells, HIV replicates and eventually destroys them, leading to a decrease in the body’s ability to fight off infections and certain cancers. As the number of CD4 cells drops, the immune system becomes increasingly compromised, which is why untreated HIV can eventually lead to AIDS.
Acquired Immunodeficiency Syndrome (AIDS)
AIDS, or end-stage HIV infection, represents the most severe form of HIV. HIV infection is classified as end-stage when an individual develops one or more serious illnesses or when their CD4+ lymphocyte count drops significantly.
AIDS-defining illnesses include.
- Opportunistic infections. These are serious infections that occur primarily in individuals with weakened immune systems. Examples include fungal infections (like cryptococcosis and Pneumocystis jirovecii pneumonia), bacterial infections (such as Mycobacterium avium complex and tuberculosis), and viral infections (including severe herpes simplex and cytomegalovirus infections).
- Certain cancers. These include invasive cervical cancer, Kaposi sarcoma, and specific lymphomas.
- Nervous system dysfunction
- AIDS wasting. Significant weight loss due to HIV infection.
Prevalence of HIV
HIV-1 first emerged in Central Africa during the early 20th century when a closely related chimpanzee virus crossed species to humans. The global spread of HIV-1 began in the late 1970s, with AIDS first identified in 1981.
By 2021, international efforts had significantly expanded access to antiretroviral therapy, with an estimated 29.6 million people receiving treatment, a significant increase from 7.8 million in 2010. These efforts have dramatically reduced HIV-related deaths and transmission rates in many countries.
In the United States, as of the end of 2021, approximately 1.2 million people aged 13 and older were living with HIV. Notably, around 153,500 individuals (13%) were unaware of their infection. In 2022, over 32,100 new HIV diagnoses were reported, with 22,400 cases resulting from male-to-male sexual contact. It is important to interpret data from 2020 cautiously due to the impact of the COVID-19 pandemic on HIV testing and healthcare services.
Globally, in 2022, an estimated 39 million people, including 1.5 million children under the age of 15, were living with HIV. Approximately 1.3 million people were newly diagnosed with HIV, down from 2.1 million in 2010, and 630,000 people died from HIV-related illnesses, a decrease from 1.3 million in 2010. Additionally, 29.8 million people with HIV were receiving antiretroviral therapy, and 86% of people with HIV were aware of their status, with 71% achieving viral suppression.
HIV infection is most prevalent in Africa, particularly in sub-Saharan Africa. In 2022, it was estimated that 25.6 million people in Africa were living with HIV, with 90% aware of their status, 82% receiving treatment, and 76% achieving viral suppression. New HIV diagnoses in Africa were approximately 660,000, representing a 66% decrease in incidence since 2010. Additionally, 380,000 people in Africa died from HIV-related causes, marking a 56% decrease since 2010.
Transmission of HIV
HIV transmission occurs when an open surface, such as a cut, in an uninfected person comes into contact with body fluids containing the virus. While HIV can be present in nearly all body fluids, transmission primarily occurs through blood, semen, vaginal fluid, and breast milk. Although tears, urine, and saliva may contain low levels of HIV, transmission through these fluids is extremely rare.
HIV is not transmitted through non-fluid contact (like touching, holding, or dry kissing) or close, nonsexual contact (such as touching a surface or object). No documented cases of HIV transmission exist through coughing, sneezing, or mosquito bites. Transmission from an infected healthcare worker to a patient is also exceedingly rare.
Common Modes of HIV Transmission
- Sexual Contact. HIV is commonly transmitted during sexual contact when the mucous membranes lining the mouth, vagina, penis, or rectum are exposed to body fluids like semen or vaginal fluids containing the virus. This typically occurs during unprotected sexual intercourse. HIV can also be transmitted through oral sex, although the risk is lower. Open sores in the mouth, vagina, penis, or rectum, bleeding gums, or contact with menstrual blood can increase this risk. Following factors can in the risk for sexual transmission of HIV:-
- Sexual contact during the initial weeks following HIV infection, when viral load is high.
- Vigorous sexual activities that cause cuts or tears in the genital or rectal areas.
- Presence of other sexually transmitted infections (STIs) such as genital herpes or syphilis.
- Injection of Contaminated Blood. HIV transmission can occur through shared needles or accidental pricks with HIV-contaminated needles. Healthcare workers exposed to such incidents have a 1 in 400 chance of contracting HIV, with the risk increasing if the needle penetrates deeply or is hollow and contains HIV-infected blood.
- Mother-to-Child Transmission. HIV can be transmitted from an infected mother to her child during pregnancy, childbirth, or breastfeeding. Without treatment, the cumulative risk of transmission is 35 to 45%. However, treating pregnant women with antiretroviral medications during pregnancy and delivery significantly reduces this risk. In areas where formula feeding is safe and affordable, mothers with HIV are advised not to breastfeed to avoid transmission.
- Blood Transfusions and Organ Transplants. The risk of HIV transmission through blood transfusions is extremely low in high-resource countries due to rigorous screening. However, the risk remains higher in countries where blood and blood products are not adequately screened. HIV has been transmitted through organ transplants when donors were unknowingly infected.
- Artificial Insemination. HIV transmission is possible through the use of sperm from an infected donor for artificial insemination. Measures, such as freezing sperm and retesting donors, have been implemented in the U.S. to reduce this risk. Washing sperm to remove HIV is another effective measure when using sperm from known HIV-positive donors.
Symptoms of HIV Infection
The symptoms of HIV vary widely depending on the stage of the infection. 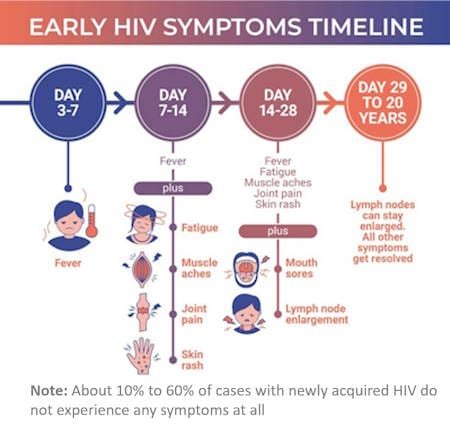
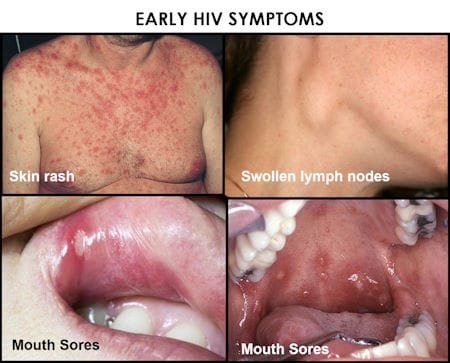
Acute HIV Infection
- Timeframe. Occurs 2 to 4 weeks after initial exposure to the virus.
- Symptoms. This stage is often referred to as primary or acute HIV infection. Symptoms resemble those of the flu, including.
- Fever
- Sore throat
- Swollen lymph nodes
- Headache
- Rash
- Muscle and joint aches
- Importance of Early Detection. During this stage, the virus is multiplying rapidly, and the body’s immune response is just beginning. Early diagnosis at this stage can significantly impact long-term health outcomes, as starting antiretroviral therapy (ART) early can prevent the virus from progressing to more severe stages.
Chronic HIV Infection (Clinical Latency Stage)
- Timeframe. This stage can last for several years, even decades, depending on treatment.
- Symptoms. Often referred to as the asymptomatic or clinical latency stage, the virus remains active but reproduces at much lower levels. Individuals may not exhibit any symptoms or only mild ones, such as.
- Fatigue
- Recurring fevers
- Swollen lymph nodes
- Weight loss
- Impact of ART. With effective ART, individuals can maintain this stage for decades without progressing to AIDS. However, without treatment, the virus will eventually weaken the immune system to the point where it can no longer defend the body against infections and diseases.
AIDS (Acquired Immunodeficiency Syndrome)
- Timeframe. Without treatment, HIV typically progresses to AIDS within 10 to 11 years.
- Symptoms. AIDS is the most severe phase of HIV infection and is characterized by a severely weakened immune system. Common symptoms include.
- Rapid weight loss
- Recurring fever or profuse night sweats
- Extreme and unexplained tiredness
- Prolonged swelling of the lymph glands in the armpits, groin, or neck
- Chronic diarrhea
- Sores of the mouth, anus, or genitals
- Pneumonia
- Red, brown, pink, or purplish blotches on or under the skin or inside the mouth, nose, or eyelids
- Memory loss, depression, and other neurological disorders
- Opportunistic Infections. At this stage, the immune system is so compromised that it can no longer defend against opportunistic infections (OIs) and certain cancers, which are the hallmark of AIDS.
Understanding Opportunistic Infections and Cancers in AIDS
Opportunistic infections (OIs) are illnesses that occur more frequently and are more severe in people with weakened immune systems, including those with HIV. In individuals with AIDS, the risk of OIs is significantly higher due to the severe damage to the immune system. Some of the most common OIs and associated cancers include.
Opportunistic Infections
- Pneumocystis Pneumonia (PCP).
- A serious fungal infection affecting the lungs.
- PCP was once the leading cause of death among people with AIDS before the introduction of effective ART.
- Tuberculosis (TB).
- TB is a bacterial infection that primarily affects the lungs but can spread to other parts of the body.
- It is the most common cause of death among people with HIV worldwide.
- Cytomegalovirus (CMV).
- A viral infection that can affect various parts of the body, including the eyes, lungs, liver, esophagus, stomach, and intestines.
- CMV retinitis, an eye infection, can lead to blindness.
- Candidiasis (Thrush).
- A fungal infection that affects the mouth, throat, and vagina.
- Oral thrush is common in individuals with AIDS and can be persistent and difficult to treat.
- Toxoplasmosis.
- A parasitic infection that affects the brain, leading to neurological issues such as headaches, confusion, seizures, and coordination problems.
- It is often contracted through exposure to cat feces or undercooked meat.
- Mycobacterium Avium Complex (MAC).
- A bacterial infection that can cause fever, night sweats, weight loss, anemia, and diarrhea.
- It typically affects the lungs but can spread to other organs in those with weakened immune systems.
Cancers Associated with HIV/AIDS
- Kaposi Sarcoma.
- Caused by human herpesvirus 8 (HHV-8), Kaposi Sarcoma manifests as painless red to purple patches on the skin, and can also affect internal organs.
- It is more common in men who have sex with men and can be life-threatening when it affects vital organs.
- Non-Hodgkin Lymphoma (NHL).
- This type of lymphoma is more common in people with HIV and can affect the brain, lymph nodes, liver, bone marrow, and gastrointestinal tract.
- Symptoms depend on the area affected but can include swelling of the lymph nodes, fever, weight loss, and night sweats.
- Cervical Cancer.
- HIV-positive women have a higher risk of cervical cancer, which is caused by certain strains of the human papillomavirus (HPV).
- Regular screening and early treatment are crucial to managing this risk.
- Anal Cancer.
- Also associated with HPV, anal cancer is more common in HIV-positive individuals, particularly men who have sex with men.
- Lung Cancer.
- People living with HIV are at a higher risk of lung cancer, even if they do not smoke, possibly due to chronic inflammation and immune system dysregulation caused by the virus.
Diagnosis of HIV Infection
Early diagnosis is crucial in managing HIV and preventing the progression to AIDS. Several tests are used to detect HIV.
- Antibody Tests.
- Description. These tests detect antibodies that the immune system produces in response to HIV.
- Types.
- Rapid Tests. Provide results in as little as 20 minutes and are often used in clinics or at-home testing kits.
- Laboratory Tests. More accurate than rapid tests, these require blood samples and typically take a few days to return results.
- Window Period. Antibodies usually develop within 3 to 12 weeks after exposure, so testing during this period may yield false-negative results.
- Antigen/Antibody Tests.
- Description. These tests detect both HIV antibodies and p24 antigen, a protein produced by the virus shortly after infection.
- Advantages. They can detect HIV sooner than antibody tests alone, typically within 2 to 6 weeks after exposure.
- Usage. Often used in routine screening and confirmatory testing.
- Nucleic Acid Tests (NATs).
- Description. NATs detect the genetic material (RNA) of HIV, making them the most sensitive tests available.
- Timing. Can detect HIV within 10 to 33 days after exposure.
- Usage. Typically used in situations where early detection is critical, such as in cases of recent high-risk exposure or in newborns of HIV-positive mothers.
Treatment of HIV Infection
Treatment for HIV involves antiretroviral therapy (ART), a combination of medications that reduce the viral load to undetectable levels, thereby preventing the progression of the disease and reducing the risk of transmission to others.
Antiretroviral Therapy (ART)
- How ART Works.
- ART involves taking a combination of HIV medicines (called an HIV treatment regimen) every day.
- The primary goal is to reduce the viral load (amount of HIV in the blood) to undetectable levels, which allows the immune system to recover and reduces the risk of HIV-related complications.
- Benefits of ART.
- Suppression of Viral Load. By maintaining an undetectable viral load, ART prevents the progression of HIV to AIDS and reduces the risk of HIV transmission to sexual partners.
- Improved Immune Function. ART helps restore the immune system’s ability to fight infections and diseases.
- Reduction in HIV-Related Complications. Effective ART reduces the incidence of opportunistic infections and HIV-related cancers.
- Adherence to Treatment.
- Adherence to ART is crucial. Skipping doses can lead to drug resistance, making the virus harder to treat.
- Many modern ART regimens are simpler and involve fewer pills, making it easier for patients to adhere to their treatment plans.
- Side Effects.
- Short-Term Side Effects. These may include nausea, fatigue, and headaches, often resolving within a few weeks.
- Long-Term Side Effects. Some medications may cause long-term side effects such as lipid abnormalities, bone density loss, and cardiovascular disease.
- Managing Side Effects. Regular monitoring and communication with healthcare providers are essential to managing side effects and ensuring the effectiveness of the treatment.
- Impact on Quality of Life.
- ART has transformed HIV from a fatal diagnosis into a manageable chronic condition. With effective treatment, individuals with HIV can expect to live nearly as long as those without the virus.
Treatment of Opportunistic Infections and Cancers.
- Prophylaxis and Management.
- Preventive Measures. ART itself serves as a primary preventive measure against opportunistic infections by boosting the immune system. Additional prophylactic treatments may be necessary for certain conditions.
- Treatment. If opportunistic infections or cancers develop, they are treated with the appropriate medications, such as antibiotics, antifungals, antivirals, or chemotherapy.
- Importance of Regular Monitoring.
- Regular medical check-ups are essential for monitoring immune function (CD4 count), viral load, and the early detection of any complications.
- Preventive care, such as vaccinations and regular screenings for cancers, plays a vital role in maintaining health.
Prevention of HIV Infection
Preventing the spread of HIV is a critical public health goal. Comprehensive prevention strategies include a combination of behavioral interventions, medical treatments, and public health policies.
Behavioral Interventions.
- Safe Sexual Practices.
- Condom Use. Consistent and correct use of condoms during sexual activity significantly reduces the risk of HIV transmission.
- Regular Testing. Routine HIV testing for sexually active individuals allows for early detection and treatment, reducing the risk of unknowingly transmitting the virus.
- HIV Education and Awareness.
- Public education campaigns are vital in spreading awareness about HIV, reducing stigma, and promoting safe practices.
- Programs targeting high-risk populations, such as men who have sex with men, people who inject drugs, and sex workers, are particularly important.
- Reducing Risk in Specific Populations.
- Tailored interventions for high-risk groups, including needle exchange programs and harm reduction strategies, are essential in preventing new infections.
Medical Interventions
- Pre-exposure Prophylaxis (PrEP).
- Description. PrEP is a daily pill taken by HIV-negative individuals at high risk of infection. It significantly reduces the risk of contracting HIV.
- Effectiveness. When taken consistently, PrEP reduces the risk of sexual transmission by about 99% and injection drug use transmission by at least 74%.
- Post-exposure Prophylaxis (PEP).
- Description. PEP involves taking antiretroviral medications within 72 hours of potential HIV exposure to prevent the virus from taking hold.
- Usage. Recommended after high-risk exposures, such as unprotected sex, needle-sharing, or occupational exposure (e.g., needlestick injuries).
- Mother-to-Child Transmission Prevention.
- Testing and Treatment During Pregnancy. Pregnant women with HIV should start ART as early as possible to reduce the risk of transmitting the virus to their baby.
- Delivery and Postpartum Care. Cesarean delivery and avoiding breastfeeding can further reduce the risk of transmission.
- Vaccination.
- Current Research. While no HIV vaccine exists yet, research is ongoing, with promising developments in various stages of clinical trials.
- Immunizations for HIV-Positive Individuals. Vaccinations against hepatitis B, influenza, and pneumococcal infections are important for people with HIV to prevent complications from these infections.
Prognosis for HIV Infection
The prognosis for people with HIV has improved significantly over the past few decades due to advancements in ART. However, the disease’s outcome depends on several factors, including the timing of diagnosis, adherence to treatment, and access to healthcare.
- Life Expectancy.
- With early diagnosis and consistent treatment, individuals with HIV can have a nearly normal life expectancy.
- The quality of life is also greatly improved, with many individuals living long, healthy lives without ever developing AIDS.
- Disease Progression.
- Without treatment, HIV will inevitably progress to AIDS, usually within 10 to 11 years. Once AIDS develops, the life expectancy drops significantly without treatment.
- With treatment, the progression to AIDS can be prevented, and the viral load can be maintained at undetectable levels.
- Challenges in Treatment.
- Drug Resistance. Inconsistent adherence to ART can lead to drug-resistant strains of HIV, complicating treatment and reducing options for effective medications.
- Co-infections. People with HIV are more susceptible to other infections and diseases, such as tuberculosis and hepatitis, which can complicate treatment and affect prognosis.
- Ongoing Research and Cure.
- Researchers are exploring various strategies to cure HIV, including approaches that aim to eliminate latent reservoirs of the virus in the body.
- Gene editing, therapeutic vaccines, and immune modulation are among the cutting-edge areas of research that hold promise for a future cure.
End-of-Life Considerations
For individuals with advanced HIV/AIDS who may not respond to treatment, or those in the final stages of life due to AIDS-related complications, end-of-life care is an important consideration.
- Palliative Care.
- Focuses on relieving symptoms and improving quality of life for those with serious illnesses, including advanced HIV/AIDS.
- Palliative care teams work to manage pain, address emotional and spiritual concerns, and support both the patient and their family.
- Hospice Care.
- For those in the final stages of AIDS, hospice care provides comprehensive support focused on comfort and dignity.
- Hospice teams offer medical, psychological, and spiritual care, helping individuals and their families navigate the final stages of life.
- Advance Care Planning.
- Discussing and documenting preferences for end-of-life care is important for ensuring that an individual’s wishes are respected.
- Legal documents such as living wills and healthcare proxies can guide healthcare providers and loved ones in making decisions that align with the individual’s values.
Conclusion
HIV/AIDS remains a significant global health issue, affecting millions of people worldwide. However, the landscape of HIV treatment and prevention has evolved dramatically over the past few decades. With early diagnosis, effective treatment, and comprehensive prevention strategies, HIV can be managed as a chronic condition, allowing individuals to live long, healthy lives.