Ovarian Cancer: Symptoms, Diagnoses & Treatment
Ovarian cancer is one of the deadliest cancers in women, in part because it is often detected at an advanced stage. This form of cancer predominantly affects women aged between 40 and 65. Globally, ovarian cancer ranks as the seventh most common cancer in women. In 2020, 313,959 women worldwide were diagnosed with ovarian cancer, leading to 200,700 deaths globally. Treatment works best when ovarian cancer is identified during its early stages.
Ovarian cancer symptoms
Symptoms of ovarian cancer can include:
- Your stomach getting bigger
- Feeling bloated or having stomach pain
- Feeling full or having trouble eating
- Needing to urinate often
When ovarian cancer begins to grow, most women may not notice any symptoms. Most symptoms usually appear at late stage of the disease.
Ovarian cancer risk factors
The following factors increase the risk of developing ovarian cancer:
- Being a white person.
- Never being pregnant.
- Early age of menarche (the onset of the menstrual periods) or late age of menopause.
- Family history of ovarian, breast, or endometrial (uterine) cancer, particularly if the person inherits a specific type of genetic abnormality called a BRCA1 or BRCA2 mutation.
- Family history of Lynch syndrome (hereditary nonpolyposis colorectal cancer [HNPCC]). Women in families with this trait have up to a 60 percent chance of endometrial cancer and a 10 to 12 percent chance of ovarian cancer.
How is Ovarian cancer diagnosed ?
If doctor suspects you have ovarian cancer, he or she might order one or more of the following tests:
- Ultrasound, CT scan or MRI – These tests create images of the inside of the body and can show abnormal growths. Radiology tests such as these do not provide enough information to definitively diagnose ovarian cancer, though they may provide important information about the location and/or extent of a possible cancer.
- Blood test for tumor markers (CA 125) – Women who are suspected of having or are diagnosed with ovarian cancer undergo a blood test to measure the level of a protein tumor marker called CA 125. This marker is normally less than 35 U/mL. CA 125 levels are elevated (above 65 U/mL) in 80 percent of women with advanced epithelial ovarian cancers.
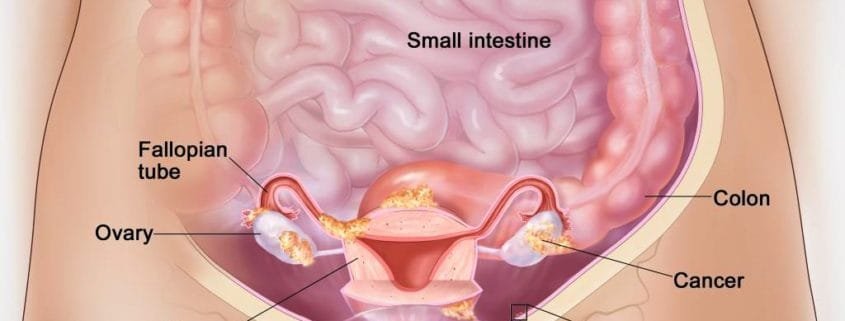
- Surgery – Diagnostic surgery is the definitive method to confirm ovarian cancer in women. During the surgical procedure, a doctor removes the affected ovary, and simultaneously, another physician (pathologist) examines cells from the ovary under a microscope to identify any cancerous presence. If cancer is detected, the surgery typically continues to address the cancer by removing as much of it as possible, known as debulking surgery. This often involves a procedure known as “total hysterectomy with salpingo-oophorectomy,” where the doctor removes not only the ovaries but also the fallopian tubes and the uterus. In cases where the cancer has spread to adjacent organs, the doctor may opt to remove those organs as well.
What is cancer staging ?
Cancer staging is a way in which doctors find out how far a cancer has spread. Based upon the findings during exploratory surgery, the tumor is formally “staged” according to the size, extent, and location of the cancer. Accurate staging during surgery is very important in determining a woman’s long-term outcome (prognosis) and choosing the appropriate treatment regimen after surgery.
The stage of an ovarian cancer is defined by a Roman numeral designation between I and IV, and subdivided by the letters A, B, and C. Generally, stages I, II, III, and IV denote the tumor’s specific location, while the subdivisions A, B, and C specify the extent of tumor involvement. A higher stage of disease signifies a more extensive level of tumor engagement.
Early stage cancer
Stage I and II disease are considered early stage ovarian cancer:
- Stage 1A and 1B: In stage IA and IB disease, the cancer is limited to one or both or ovaries, and the capsule or membrane covering the ovaries has not been broken by the cancer’s growth.
- Stage 1C: In stage IC disease, the capsule of either ovary may have ruptured or there may be signs suggesting that cancer cells have begun to spread within the pelvis (ie, there are cancerous cells in the fluid taken from the peritoneal cavity during surgery).
- Stage II: In stage II, the tumor involves other pelvic organs, such as the uterus or fallopian tubes. Early signs may indicate potential spread beyond the pelvis.
Advanced stage disease
- Stage III: The cancer is confined to the abdomen and abdominal lymph nodes.
- Stage IV: Cancer has spread to distant sites such as the liver or lungs.
Ovarian cancer treatment
For most women, the initial treatment involves surgery to remove the cancer. Further treatment depends on the cancer stage, a woman’s age, and other medical factors. Some may not require additional treatment, while others may undergo chemotherapy, a group of medicines that target and eliminate cancer cells.
Fertility Considerations: If you aspire to conceive in the future, inform your doctor before undergoing treatment. Ovarian cancer treatment often results in infertility, but in some cases, it might be possible to plan treatment to preserve the possibility of pregnancy.
Post-Treatment Monitoring: After treatment, regular check-ups are essential to monitor potential cancer recurrence. Follow-up tests include blood tests, physical examinations, and imaging. Being vigilant for symptoms is crucial, as their recurrence could indicate a possible return of cancer. Report any symptoms promptly to your healthcare provider.
What if I want to get pregnant in future ?
If your future plans include starting a family, communicate this desire to your doctor before initiating treatment. Ovarian cancer treatment often leads to infertility, but for certain women, it might be possible to plan treatment so that pregnancy is still possible.
What happens after treatment?
After treatment, you will be checked often to see if the cancer comes back. These follow-up examinations typically include blood tests, physical exams, and imaging tests. It’s crucial to be vigilant for the symptoms mentioned earlier, as their reappearance may signal a potential recurrence. Promptly inform your healthcare provider of any concerning symptoms.
What happens if the cancer comes back or spreads ?
In the event of cancer recurrence or spreading, additional options may include more surgery, chemotherapy, or a targeted therapy medication designed to inhibit cancer growth.
Can ovarian cancer be prevented ?
If ovarian or breast cancer runs in your family, talk to your doctor. There may be things you can do to keep from getting cancer.
Ovarian Cysts vs. Ovarian Cancer
Ovarian cysts are common and can be concerning, leading to worries about ovarian cancer. However, it’s important to understand that having an ovarian cyst does not mean you have ovarian cancer. Ovarian cysts are fluid-filled sacs or pockets of regular tissues, while ovarian tumors are solid masses of cancer cells. Most ovarian cysts come and go with menstrual cycles, whereas tumors require treatment. Although some symptoms of ovarian cysts can resemble those of ovarian cancer, most cysts are harmless and don’t indicate an increased risk of future cancer. However, complex ovarian cysts may raise the risk of cancer, particularly in older individuals. It’s essential to seek further understanding of ovarian cysts, their formation, and when to consult a doctor. It’s important to ask questions and seek a second opinion if concerns are not adequately addressed or taken seriously.
What else should I do?
It is important to follow your doctors’ instructions regarding visits and tests. Open communication about any side effects or challenges during treatment is equally important. Making decisions about ovarian cancer treatment involves numerous choices, and your input is valuable. Always express your thoughts and feelings about a treatment, and don’t hesitate to ask following questions when considering a new treatment option.
- What are the benefits of this treatment?
- Is it likely to help me live longer? Will it reduce or prevent symptoms?
- What are the downsides to this treatment?
- Are there other options besides this treatment?
- What happens if I do not have this treatment?